CHAPTER 8
Systemic Design for Healthcare Innovation
Elena’s Story: A System Upgrade
Elena returns to the cardiac care center 2 weeks after her scan and diagnostic procedures. She maintained her medication schedule and her rapid heart rate did not return, so now she wonders whether the invasive procedure is really needed. She has second thoughts about agreeing to what feels like an extreme procedure.
Elena arrives at the center at 6:30 a.m. for her appointment with electrophysiologist Audrey Chen. She is greeted by a receptionist, signs insurance and consent forms, and waits briefly. Unlike at the hospital, she is immediately escorted to a prep room by a staff nurse. Elena changes into a flimsy green gown, and the nurse takes vital measurements and discusses the radiofrequency ablation procedure.
Dr. Chen must first initiate diagnostic testing to “map” the arrhythmia. After administering local anesthesia at the catheter entry points, she inserts a needle through Elena’s right femoral veins leading up to the right side of the heart. A sheath is run over the needle to guide the catheter’s entry, using a fluoroscopic display to guide the ablation needle. Three catheters are introduced to the bundle of His near the aorta, at the right side of the heart. Dr. Chen electrically stimulates several critical points of the heart’s circuitry with the catheters in an attempt to reproduce the kind of arrhythmia Elena has spontaneously generated. She looks for the patterns in the real-time ECG to determine when she has reproduced the SVT signals.
Once the arrhythmia is reproduced (a complex process that can take well over an hour), Dr. Chen maps this electrical circuit by locating the nerve signaling positions on the heart. After confirming with the ECG reading, Dr. Chen inserts the ablation catheter through an incision in the groin. She guides it to the heart location using the ultrasound display from a second catheter that monitors the ablation. The ablation catheter is controlled to deliver radiofrequency pulses at selected points in the heart tissue.
Dr. Chen proceeds to “ablate” (electrically cauterize) the absolute minimum that is necessary to stop the arrhythmia. The ablation instruments are powerful and can literally burn a hole in the heart, a potentially catastrophic complication. The entire procedure, from catheter insertion to post-operative recovery, is about 6 hours for Elena’s case.
Elena has no way of judging the quality and sustainability of her treatment. As long as the SVT symptoms do not reappear, she has no way of knowing how her body has accommodated the treatment.
There are hundreds or thousands of small errors that could occur in the diagnosis, mapping, and ablation procedure. The fact that the vast majority of ablations are performed without problems during or after attest to the high level of training and the level of trust in the standard of care.
Elena’s ablation is an advanced technical procedure that is fully dependent on formal institutional practice. The clinical focus on body systems (e.g., cardiovascular system) translates biomedical research and advances in procedure into innovations for specialized care. The body-system orientation facilitates the development of specialist expertise, but reinforces a tradition of problem-based, not person-centered care.
A successful procedure reinforces the perception that optimal health outcomes have been achieved. It suggests that service delivery is value received, when value is only realized upon improved health as declared by the customer, the health seeker. In many specialist care situations, patients may not realize that other valid therapeutic alternatives may be possible. Between the high-cost standard of care (a business driver) and the customer’s knowledge gap, there may be little motive to change the model of care.![]()
Disruptive Transformation
Innovation theories celebrate the value of “disruptive” innovation as the most competitive form of innovation. Business authors claim disruptive interventions have the most impact and profit potential, because disruptive entrants displace winners in large economies. Disruption of current practices has become an aim of innovation, if not its very definition. Disruptive or radical innovation promises rapid change with technological inter-ventions—yet healthcare systems are designed as institutions, which are resistant to any type of rapid change.
In healthcare practice, the goals of transformation are perhaps more relevant than disruptive innovation. US healthcare and other publicly financed systems face a long-term cost and financing crisis as populations grow, age, and use more healthcare services than are supported by revenues. A large proportion of healthcare services are “delivered” from a centralized care model in which people visit a regional hospital to have emergent or acute problems treated. Yet common chronic illnesses such as acquired diabetes, metabolic syndrome, and asthma are becoming pandemic, and there are no easy design solutions for prevention or intervention at the societal scale.
Innovation in Markets or Services?
Clayton Christensen1 defines disruptive innovation as the way smaller entrants grab a niche market by offering similar products at much lower cost. Or by providing a single significant feature overlooked by current users, they build a new market that leapfrogs the competition. They eventually overtake established players when their offerings expand to fulfill the larger demand of the market as their value proposition catches on.
We often celebrate innovation for its own sake. But in healthcare, we might be more cautious about the intent of innovation:
• What exactly is being “disrupted”?
• Is a disruptive or radical innovation the right mindset and frame of reference for healthcare innovation?
• Whose values are being optimized when technology is hailed for “disrupting healthcare”?
• Are we learning from the vast history of technology and software failures and unintended consequences in healthcare applications?
• Is new necessarily better, or is any chance to improve good?
Even if many healthcare services are profit-based, should innovation best be envisioned as enabling a competitive outcome? It depends on the market being disrupted. In the care market, human lives are at stake, not merely profits. If the market is competing products in the healthcare industry, then disruption or radical innovation may lead to market share dominance. But new products more often incrementally improve well-known care practices than transform them. They maximize care while incurring minimal risk in their adoption.
CT and MRI imaging systems were breakthrough innovations and transformed diagnostics and surgical outcomes by significantly improving diagnostic imaging. Yet even these powerful diagnostic systems—together considered the top medical innovation of the last 50 years—did not reinvent the hospital, streamline inpatient care, or even change clinical workflow. The da Vinci minimally invasive and remote surgical system is one of the newer significant innovations of both technique and workflow. Yet the system does not replace a surgeon’s skill as much as it improves options for the patient, with less-invasive procedures and robot-assisted remote operations.
Breakthrough treatments or techniques that transform healthcare services are not disruptive to clinical work in the economic sense of innovation. For example, a new entrant may introduce an innovation into a competitive market, such as the pen-style insulin injection systems for diabetics. The new Timesulin pen cap (Figure 8.1) adapts to pens already in the market and displays the last time of injection. It solves a single problem well.
The Timesulin approach disrupts the competition among insulin devices by providing a better product unavailable from the current providers. Though it does not disrupt clinical care, it disrupts the product ecosystem by improving a necessary application by adapting to the most current accepted innovations already in the market.
FIGURE 8.1
Timesulin insulin pen cap. (Courtesy Marcel Botha, Timesulin)
The healthcare system absorbs new technology and prices it into the existing delivery model. New care services are adopted if they are shown to be effective and are supported by evidence, even if they cost more. New services in sequential care modes (such as continuing services for diabetes, allergies, dialysis) have direct patient impact, but may raise costs when first implemented. New services in iterative modes (chronic, cancer, cardiac) may not be seen as novel by patients.
Because patients often receive a specific type of treatment only once, they may not be informed or repeating customers. They have little to compare, even if their treatment represents a demand and its fulfillment represents received value. Thus the patient experience of a healthcare innovation may be invisible. The radical improvement is only appreciated by its absence and is perhaps measured by not noticing. If a service innovation helps the clinical team maintain awareness, sensitivity, and control over a difficult procedure, the invisible value may also be recognized in the errors or lengthy duration that did not occur due to an improved clinical system.
What Is the Target of Innovation?
Reliance on a profit-based business model in healthcare and its supplier industries (pharmaceuticals and IT in particular) has resulted in the expensive, fragmented, and unsustainable US healthcare system. Insurance firms and health maintenance organizations (HMOs) have less incentive to innovate because they have established regional monopolies and have little organic competition. The obvious entry of government as a global underwriter and single payer would disrupt the noncompetitive insurance model.
Although some observers propose that changing market incentives to enable an even freer market of payers could result in fair competition for healthcare business, new entrants are at a serious disadvantage. The entrenched provider-payers enjoy a privileged position; they have influenced policy for decades, have deep pockets to compete with low-cost models, and own proprietary sources of patient data for analyzing risk and underwriting. The insurance model establishes a very high barrier to entry.
The core innovation problem at this level is not the disruption of service models but the transformation of payment systems. There may be no perfect system anywhere, but the US system is uniquely structured to prevent universal care and institutional innovation.
Healthcare policy reveals cases of unwanted, anti-innovative disruption. The insurance industry has by default designed the healthcare delivery system in the United States by mediating payment for care procedures. As policies are instituted to give more oversight of patient services and payments, significant consequences to costs and everyday clinical management will arise, often moving the system in the opposite direction intended by decision makers. The planned implementation of the ICD-10 coding system (with tens of thousands of finer-grained billing categories) will require system-level updates to all US billing and electronic medical record (EMR) systems that track and code medical procedures. Although the standard was intended to enable better cost oversight, ICD-10 will be disruptive, costly, and counterproductive.
The need to account for piecemeal billing has led to fragmented procedures, as clinicians must keep track of every micro-task that could possibly vary for billing and reimbursement. This creates a significant overhead to track, account for, and defend every procedure on a bill. This pressure places perverse incentives on clinicians to identify variants that can be reasonably reimbursed, not to extract from the payer but just to break even with legitimate time spent in clinical consultation. (In US healthcare, there is no way to bill for the procedure known as “conversation.” My Canadian family physician spent two hours in conversation with me on our initial intake to the practice. Our appointments have never been rushed for time. Though there are many other contrasts, the ability of Canadian doctors to cultivate a personal understanding is something most US patients may never see.)
There are hundreds of possible targets for innovation, but few have an effect on the system or organization as a whole. A systems view of innovation considers the whole system and its interrelated components. Innovation or disruption is efficient and influential when the least effort has the largest desired effect. Although social systems such as healthcare practices are dynamic and change may not be predictable, there are systems and design methods that enable stakeholders to determine the maximum benefit or influence in innovation or change programs.
The Healthcare Innovator’s Challenge
The innovator’s challenge is to understand and preserve core values while changing practices for durable social and economic benefit. Although economic value is often a pivotal driver of innovation adoption, cost management is not itself a core value but a sustainability factor to be evaluated in decision making. The related social innovation challenge is perhaps a macro policy problem, not a design issue. A significant social impact from cost savings could be obtained from transferring value from a high-profit sector to facilitate better access to services and improve primary care.
Healthcare is a social and public good that can be provided universally, in some form, as in most developed countries. In the United States, this would require a truly disruptive change to public policy and the insurance payer model of the healthcare system. As a recent New England Journal of Medicine article declared,
It is hard to ignore that in 2006, the United States was number 1 in terms of health care spending per capita but ranked 39th for infant mortality, 43rd for adult female mortality, 42nd for adult male mortality, and 36th for life expectancy. These facts have fueled a question now being discussed in academic circles, as well as by government and the public: Why do we spend so much to get so little?2
Was there ever a clearer innovation challenge in any sector or business? Healthcare as an industry faces multiple crises that beg for systemic solutions, not piecemeal fixes. System interventions aim for the root issues most closely related to the perpetuation of critical problems. Sustainable solutions are those that economically scale across institutions and regions.
Systemic redesign requires agreement on a shared vision of the future value state. Any project aiming to satisfy multiple stakeholders (not just users or owners) requires a systemic approach, rather than the mere negotiation of service functions. We might reframe the purposes of “disruptive innovation” in institutional healthcare from economic and technical value to that of co-creating significant service transformations that benefit all stakeholders.
Systemic Design in Healthcare Service
This book maps to three systems: the individual health seeker, clinical practice, and institutional healthcare. Each is a complex system with different opportunities for system change resulting from services within the system. The design and research methods appropriate to one system context may not transfer well to the others.
Systemic design adapts design practices to sociotechnical complexity. By integrating systems thinking and its methods, systemic design adopts human-centered design to co-create complex, multistakeholder services such as those found in medicine and healthcare.
Any system is an emergent network of deeply interconnected functions that achieves an intended purpose. Every system can be seen as social or human-influenced. Systems researchers report consensus that human intervention has touched all aspects of the planetary ecology. As a result they call our current era the Anthropocene. So we can also say “all systems are social.”
Systemic behaviors occur throughout healthcare. Systems (including most medical services) may fail in unpredictable ways if their components are separated from the connected whole. Cases show traditional product development approaches to innovation often fail in a complex system scenario. As planners and designers, we focus on the wrong object for innovation, often expecting an IT application to diffuse into an organization with intended system-wide uses. In complex sociotechnical systems like medicine, the planned adoption becomes fraught with challenges, and the unintended effects outweigh the benefits.
A Systems View of Specialty Medicine
The shortfall of US primary care practitioners is a systemic case. Growing from a primary care crisis into a permanent situation, it has evolved into the current specialist-based dominant system. From a systems perspective, specialists create a market of specialist health problems, which satisfy the demands of the “big box healthcare” business model. As the rights to certain procedures are owned by specialists, primary care physicians become busy brokers of referrals to the specialty system.
The specialist body-system model fulfills its intended purposes well—patients with broken hips see orthopedic surgeons, cancer patients see oncologists, cataracts are treated by ophthalmologists. However, the clear societal need in the United States and other national systems is for more accessible primary and preventive care. If primary care were more successful, it would greatly reduce the need for highly profitable specialty services.
The vast majority of all physician encounters are for outpatient treatment, whether specialty or primary care. Medical residencies have prepared trainees for inpatient care at the expense of societal needs. A recent Johns Hopkins study showed that residents trained in community hospitals were better prepared for basic outpatient care than those in the large academic medical centers where most residents are trained.3 The status and monetary bias toward specialization may prevent many of the best doctors from going into primary care service. This bias is a positive feedback loop that produces more of the same outcomes over time.
Consider Elena’s scenario in this chapter. Her patient experience could be enhanced in many ways to reduce anxiety or facilitate quicker restoration. If her ablation procedure works as intended, is there any payoff for clinics to make incremental improvements in short-term care experience?
Specialist care is necessarily reactive, based on referrals and responding to disease discovery, and is not positioned to proactively prevent health problems. From a preventive care view, specialists are counter-systemic, as their service waits until illnesses erupt into obvious health concerns. Even specialized medical tests are often counter-systemic, as aggressive testing often leads to unnecessary procedures. Specialists (and surgeons) are also not institutionally able to engage patients as whole persons with multiple life and health issues. This may prevent individuals from understanding and tackling the root causes emerging from their lifestyle and behavior. The specialist model has no systemic incentive to deal with underlying root causes, as prevention or mitigation could reduce specialists’ income growth. Given the insurance-based payer model, the specialist is incentivized to conduct as many high-paying procedures as possible.
This is not an indictment of specialists. The need for specialty care has also increased with population growth and aging, and with the advancement of technical procedures. Their maximization of profit by procedure type or volume is entirely rational. Proposing radical innovations to their established model will encounter cultural resistance from the current system. Technological innovations (such as the ultrasound-guided cardiac procedure Elena undergoes) do not usually reduce costs but yield clinical goals, easing invasiveness and increasing reliability and sophistication.
Primary care physicians usually have significant patient caseloads and are unable to actively follow referred patients, at least until follow-up. The family doctor is not part of a collaborative care team in the inpatient context, and may only be copied on the clinical report and final ECG after treatment. Continuity represents a major service and IT design challenge for the foreseeable future, even as EMRs become integrated across practices. If a new role of care coordinator was introduced across the patient’s entire disease cycle—from diagnosis to aftercare consultation—a whole-care experience could be co-created with the patient’s health-seeking journey. The patient experience is directly improved by such continuity.
A systemic design considers the entire flow of specialist service. Specialists are not typically trained to engage the whole person or a holistic view of treatment. In fact, in Elena’s entire health-seeking journey, no single clinician or coordinator attends to all her treatments and medications. Known as continuity of care, in multi-condition, multi-specialist situations, a holistic coordination of treatment and medication is, unfortunately, quite rare. It is also a huge opportunity for innovation, as presented in the IDEO case study in Chapter 6.
Chronic disease exposes the systemic weakness of the specialist model. Environment- and lifestyle-induced diseases such as diabetes and cancers increase in the population and complicate any other conditions. Multiple treatments and medications are costly to providers and society. Unraveling these causal impacts is difficult because each is also an effect of other long-term causes, such as environmental degradation and the marketing of unhealthy lifestyles. Unfortunately, the current US market-based system provides no incentive or process for managing multiple combined conditions effectively.
Systemic Innovations in Primary Care
The specialist model will not be changed “by design” because it is profitable and institutionalized. Even minor changes will trigger lobbying in response to policy design. Disruptive change will emerge from innovation on the input side, by reducing the referred patient demand to the specialty practices.
Practice innovation is motivated by business and operational structure more than clinical process. Integrated practices combining primary care and related specialties are growing, as their cost and business models adapt more quickly to changing payers and incentives. Among these new structures are the accountable care organizations (ACO), the manifestation of a major policy innovation emerging in the United States from the 2010 Affordable Care Act. These are decentralized and cooperative clinical practices that promise better cost management and quality care, usually connected to a traditional hospital system or payer network. ACOs are envisioned as evolving toward community-located or distributed health clinics that promote a community-oriented, patient-centered model of care. ACOs are “accountable” in that their risk and reward is based on a defined segment of their population, to which they are responsible for measures of community health and quality goals. Though the ACO is a policy innovation, the result will be a rapid evolution of new clinical business models, allowing innovative practices to experiment with approaches that fit their community needs. The model encourages a coordinated care approach for patients with complex and chronic diseases and for the predominant concerns of a community area.
The ACO model is community-based, not regional, yet it is growing in large urban areas, establishing a cooperative ecosystem with hospitals. According to a 2012 study, 221 ACOs are in operation in 45 US states, primarily in larger urban areas.4 Most ACOs (67%) are private, single-provider groups comprised of cooperating generalist, primary care, and relevant specialists providers. The growth of ACOs has been largely based on the favorable risk and payment model provided to early adopters.
Another structural innovation is the alternative primary care model, the patient-centered medical home (PCMH). Promoted by the Agency for Healthcare Research and Quality and other foundations and organizations, the “medical home” concept is not home-based care but rather a compact community health center with strong support for localized patient-centered care. The idea has been developing since the 1960s, but has only recently caught on as an alternative practice model. The new PCMH model has a triple aim of quality, improved patient experience, and lower costs while directing the practice toward a personal physician with coordinated and continuous care, a whole-person orientation, and a wider range of communications approaches. The medical home and ACO models have rapidly changed the organizational environment favoring institutional innovation.
To Innovate, Follow the System
Patient-centered service design does not aim for a “user experience” but rather health outcomes. Health outcomes are realized at some indefinite point after care services and self-care, and are both measured and experienced future benefits. Outcomes can be seen as an emergence of many design inputs, most of which are invisible to the patient.
How can innovators move clients beyond the current entrenched system? In commercial healthcare (pharma, HMOs, insurance), we unwittingly maintain the current system when extending a dominant position in a market. Even enhancing service (patient-centered or otherwise) within the established business model almost always reinforces the current system and denies system change. Adapting design to improving current service for large, profit-driven organizations may only sustain the injustices of financially driven healthcare. Design thinking, even when “challenging the brief,” does not challenge the assumptions of business logic and client economics.
Who is empowered when we design better ideas for clients that benefit from the current system? Our clients will not endorse a scope that aims to disrupt the very system that sustains their revenues and supports their ongoing role and business. Many of these opportunities may be disguised by the rhetoric of “care” and “patient centeredness.” The contributions of service design may extend and even lock in regressive practices by making them accessible and easier to use.
Fixing the wrong thing well is a typical system conundrum. Although systems thinking excels in finding ways to navigate complexity, the systems disciplines integrate very few design methods. And design-thinking methods—including fundamentals such as cyclic iterations of prototypes, human-centered design research, and shifting problem-solving contexts—are insufficient by themselves in complex systems.
Systems thinking includes science and design, which both must converge to design social systems. In systems thinking, the organization is regarded as a high-leverage target for system change because organizations are functionally coherent and purposeful. Policies and roles can be changed directly. Leverage points for changing behaviors can be defined within the organizational system. Changes to internal medicine practice (as in this chapter’s case study) have impact across the clinic and all services that draw from the practice. If a large organization succeeds in a systemic change, the new process has significant leverage across the sector as an exemplar.
Organizations are social systems that stakeholders can directly influence and design (the purpose of Design 3.0). Yet organizations are never whole systems as they exist to serve a customer or community, which participate in social (D4.0) and economic ecosystems. The organizational boundary is a powerful frame, so it is typical for innovation teams to ignore the whole system beyond the hospital or the company.
The Four Systems of Healthcare
A “system” can be defined as a purposeful collection of interdependent activities that operate as a single dynamic and complex process, with intentional or automatic regulation over its inputs of resources, energy, and information to produce defined outputs. In any whole system, the parts are inextricably interdependent and the whole has a single identity.
Wharton management professors and systems thinkers Jamshid Gharajedaghi and Russell Ackoff developed an integrated foundation of systems and design thinking spanning several decades. Gharajedaghi articulated five essential qualities of systems that designers can account for:
• Purposefulness
• Emergence
• Openness
• Multi-dimensionality
• Counterintuitive behaviors5
Many different system types can be articulated, but for the purposes of system design, we require a reduction of variety to make choices. Ackoff defined a simple four-system model based on whether the whole system or its parts exhibit intentionality, as a way to call out the critical complexity in social systems.6 For healthcare, the four systems can be viewed within the single context of a large urban clinic as the patient, the EMR system, a hospital, and the city or geographic region it serves (Table 8.1).
TABLE 8.1 ACKOFF’S FOUR SYSTEM MODELS
System model |
Parts |
Whole |
Real system |
Deterministic |
No choice |
No choice |
EMR application |
Animate |
No choice |
Choice |
Patient |
Social |
Choice |
Choice |
Hospital |
Ecological |
Choice |
No choice |
City |
The connection may be closely drawn from Ackoff’s systems to the four design geographies of D1.0–4.0. In general, the design orientation to each system level maps as follows to the four levels of clinical design:
• CD1.0: Traditional design for mechanistic IT and communication systems (billing systems, wayfinding)
• CD2.0: Products and services design for human systems (medical devices, typical healthcare services)
• CD3.0: Organizational design for well-bounded social systems (practices, hospital departments, ACO)
• CD4.0: Social transformation design for ecological systems (community, policy, health system level)
The four systems are reviewed briefly for each relationship.
Deterministic Systems
Few systems in reality are purely deterministic (or mechanical), especially in healthcare, whose systems are entirely organized around human health. All communications, products, and materials are designed for interaction with a human health context, implying some choice in the use of the system. Generally deterministic systems are defined by their structure and interactions from external functions. Health IT, from Web apps to enterprise EMRs, can be seen as mechanistic in their operation—without human intervention, they exhibit no purposeful choice, and they are determined by their programming. The skills and mindset of mechanistic systems applies to both design and system functions for this level. The highly reliable implanted pacemaker, for example, is a mechanistic medical device designed as a closed system, fully functional once programmed, needing minimal monitoring or control. Although these mechanisms are devices for human systems, they do not function like animate systems.
Animate (Human-Centered) Systems
A human being is a whole animate system with choice as a whole, in which components (body systems) have purposes but no choice. Here the human system is an agent interacting with the environment and making choices with respect to physical, objective feedback from the world. Human-centered design often covers both animate and social systems without distinguishing between them. When healthcare service is treated as a traditional body-centered model of the patient, an animate system viewpoint is implicit.
When a human is conceived as acting within a sociotechnical system, as a person in other words, his or her role elevates from animate agent to a social actor. The patient-centered care model is an attempt to integrate the patient as a whole person, but it often falls short of the social system ideal. By idealizing a patient’s experience, the system is bent to meet the symptomatic, medical, and customer needs as perceived by given human actors. The measure of quality is dependent on an underinformed participant in a complex system (even if patient health is the desired outcome).
Social (Organizational) Systems
Social systems are purposeful, persistent, human-constructed, and highly interconnected networks of processes, activities, rules, and actors. Hospitals are social systems that serve the communities within a geographic region and are constructions of policy, practice, and organizations. Universities, medical schools, clinical practices, and families are all social systems. All services are social systems, whether or not they are defined as such by service designers and client teams. Any organized entity involving multiple stakeholders constitutes a social system, with choice at both part and whole levels of action.
Social systems are designable from both design and systems methodologies. Organizational systems (with the neat boundary of the firm or institution) are researched and redesigned within the frame of D3.0 skills and processes. Open societal systems, nongovernmental organizations (with no defined boundary), and many policy organizations are framed by D4.0, a social transformation approach to change rather than a design-led methodology.
Sociotechnical systems are a type of social system developed in the healthcare research literature. They are defined by dynamic, mutual interdependence among socially organized subsystems (people, their activities, roles, and relationships), technical subsystems (information technologies, practices and techniques, workflow, work settings), and organizational environments. The unit of design and analysis of the sociotechnical system is “the system,” although technical activity and workflow are often directly studied to assess and redesign technologies and the underlying social systems.
Ecological Systems (Ecosystems)
Ecological systems are the most complex systems, as they are living systems and subject to interventions of the choiceful systems (animate and social systems). Ecologies respond in a determined causal way (as a whole) to interventions such as animate activity, human outputs, natural forces, and the dynamics of living beings that depend on the ecosystem. Their components are both living systems (humans, animals, plant life) and social systems, and the activities that characterize the ecology as dynamic are largely the choices of these part-subsystems. They are considered extremely complex largely because of their emergent and adaptive behaviors in response to a myriad of inputs, which cannot be predicted by human observers.
The colloquial reference to “ecosystem” as a constellation of interdependent social and technological services should be treated metaphorically. The social ecosystem is just a larger social system, considered as the largest boundary of systemic design action at the D4.0 level.
Encountering a Mess of System Problems
There is no single “whole system” in healthcare identified by a boundary such as “the US healthcare system.” Instead, there are many whole systems, most of them overlapping in function, that represent different social systems. Incremental improvements to these service systems may have significant positive impacts on the performance of the whole.
Each system type is identified and innovated differently by design, management, and engineering disciplines, leading to the confusion of distinctions that occur when we discuss design in healthcare. For example, the information systems mindset of health IT orients toward deterministic systems in research, design, and methodology. EMR teams rarely include social scientists or design researchers, and workflow is usually defined as a standard, not a cognitive task. Designers make the mistake of viewing breakdowns and observed frustrations as service design requirements. By elevating the patient “customer” to a sacred construct, systems are designed to produce an optimized experience. However, a service systems approach might sacrifice parameters of patient experience with a life cycle–oriented service strategy that designs for better overall value in realized health outcomes.
Service systems, even if not “designed,” function as whole systems. The integration of IT, technical practices, and organizational dynamics becomes shaped into a coordinated, emergent process more powerful than the sum of its parts. The emergent character of these functions operating as a whole creates a resilient, productive system that resists “disruption” as innovation theorists like to imagine. However, small changes to critical functions, so-called high leverage interventions, can result in new practices that become unintentionally innovative.
In real terms, intervention in one system often excludes valuable expertise found in the others. The most widely used health records systems are mechanistic—they regulate policies by encoding business rules, billing codes and related forms, and of course, patient records. Social systems within the clinic are largely ignored and are even replaced by “big data.” EMRs are not designed for the proactive provision of deep local knowledge of specialized practices, or knowledge of patient and care communities served, or even local practice management.
Consider the obvious “problem” of wait times in care service, such as surpassing target wait times for emergency room patients. Wait times are an effect resulting from a mess of interacting causes. These causes may differ between institutions and even departments—therefore even a hard-won analytical solution to “the problem” may not transfer to other institutions.
When we measure effects as problems, we point to underlying systemic issues. Our problem-solving practices (which include design) are often constructed to produce the right measure, not to achieve the underlying goal the measure was designed to indicate.
Even with obvious gaps in medical knowledge, designers bring a valuable perspective to clinical and social health problems. Design thinking changes the context for rational problem solving by constantly reframing with stakeholders who may have settled early on “solving the wrong problem.” Solving the right problem—or more accurately, finding a better problem—may be design’s most important contribution.
Can Systems Care?
We call situations “problems” because they raise shared concerns triggered by values. Problems may not have a common basis in fact or even agreement. They may appear to have existence and their resolution may reduce uncertainty, but all are matters of interpretation.
Many of the problems in healthcare are recognized by their visibility rendered by valuing care (as opposed to efficiency, for example). Values of care are responsive in all “choiceful” system types in which humans are involved—animate, social, and ecological. Only individuals (or beings with choice) can be said to care. Families, communities, and organizations of all kinds are social systems designed for caring for those within the system. The smallest social system, the couple, is also a mutual circle of care. Circles of care are formed as purposeful micro-social systems to facilitate caring and health seeking among a small collective.
Social systems can be designed for providing and reinforcing care, as a preferred or idealized value in the world. Social systems designing requires a design process quite different from products and artifacts. CD4.0 is informed by assembling stakeholders from across organizational and community perspectives to formulate an understanding of values and purposes to develop a strategic frame.
The formative social systems thinkers (e.g., C. West Churchman, Stafford Beer, Alexander Christakis) created system methods that start with understanding stakeholders and their fundamental values and purposes. Social systems design follows laws of systems science. A primary law is cybernetician Ross Ashby’s principle of requisite variety: the variety of the control system must be equal or greater than the variety of the system being controlled. Social systems design adapted this cybernetics principle by increasing stakeholder diversity (with their domain experience and personal knowledge) in place of controls and feedback loops. Social systems design follows a democratic design philosophy, embracing the diversity of roles, power, practice, values, and risk to design services that all stakeholders in the system can support.
People extend their values as systems of caring into ecologies and for inanimate objects and machines. Individuals and organizations care about their technological choices and the tools and materials associated with practice. We devote care for natural ecologies in our immediate locales and across the planet. The human capacity for empathy can be extended to things as well.
Business Models as Values Systems
Values are enduring preferences that guide personal and organizational behavior, decision making, and managerial action. Values embed tacit knowledge and they perform the same function as knowledge—they are beliefs that enact what we understand to be true and worthwhile. They efficiently move us to act on priorities without the need to pause for deliberation or reflection, as would be expected when values conflict with other organizational demands.
Organizational values are not the inspirational messages printed on wall posters. They are normative rules that encode collective preferences and desired states, and result in hiring decisions, budgets, major investments, internal agreements, and community initiatives. Values systems function systemically, as a network of interdependent values that emerge as a whole, often recognized as “the way we do things here.”
Real values are built in to business models and routine processes, each of which have values systems. A hospital’s emergency department operates from different values than the IT or clinical research departments.
A hospital’s business model acts as a process guideline and arbitrates values conflicts when they occur. Hospital business models generally reflect values in use, which are typically grounded in efficiency and safety. If we intend to innovate the institution, the business model is the place to start. The dominant logic of the clinical enterprise is a centrally managed collection of independent service lines. If the hospital was organized as a service system with a distributed logic, enabling cooperative services, staff, and payment across business lines, a whole-system approach could develop. New business models follow the development of new service lines.
Business models are artifacts, whether formalized or not, that are designed by management as road maps of intra- and interorganizational relationships and their commitments to people, resources, and economic logic. Business models serve as maps of the decision territory for organizational stakeholders to identify relationships between contributing resources, customers, and revenues. Ultimately, business models are planning tools for effective design of an enterprise social system.
The business models of care organizations can be reenvisioned to formalize agreement on the partnerships and operational processes that ensure the well-being of patients, providers, and the served community. However, business models rarely consider the strategic value of the ecosystem (natural capital, water access, air quality) or the health value of a region’s environmental management. In fact, most hospital business models overlook the necessity of accounting for social sustainability, providing resources for improving health access, and equity. Urban medical centers embrace social welfare in their outreach and community partnerships, and are becoming responsive to social needs for home care, community awareness and education, transportation, and health hazards. Yet even these core social functions are not yet strategic services in the organizational business model.
Leading healthcare centers in the near future (within 5 years in progressive cities) will begin exploring sustainable business models beyond the current “triple aim” strategy of care, health, and cost.7 (They will have to develop new business models because the big box healthcare facility will be seen as a relic in roughly 5 to 7 years.) A new triple aim of strongly sustainable business models will encourage organizational design and accounting for financial, social, and environmental well-being, beyond individual care satisfaction. The new community-based clinics are well positioned to design and champion novel business models to lead the sector. They have a historical opportunity to lead health and other service sectors in a moral and social transformation of healthcare service systems as sustainable community-led enterprises.
We know that poorly planned neighborhoods, mediocre education, inadequate public transportation, and unregulated food and water sources all contribute to poor health outcomes in the near and long term. The public centers of health and research have the position and influence to promote community-level health, and can sponsor the alignment toward new value systems for ecological and social capital.
Patient-Centric Design Values
The patient-centered care movement started as a way to relocate the appreciation of the patient from a “case” in the clinic to the central meaning of care. Though perhaps nursing has always been patient-centered, the slow change to patient-centricity across medicine has emerged from strong advocacy, education, and most critically, designing care services in ways that respect the needs of the whole person.
Patient-centered care was succinctly defined by Don Berwick of the Institute for Healthcare Improvement as “the experience (to the extent the informed, individual patient desires it) of transparency, individualization, recognition, respect, dignity, and choice in all matters, without exception, related to one’s person, circumstances, and relationships in health care.”8
How might service designers act on these values? As care services continue to align toward these guidelines as moral anchoring points, we will observe situations in which values conflicts emerge and we may also have to make choices. “Choice in all matters” as a principle affects every touchpoint.
Patient-centered medicine has developed into a meaningful and desirable value system in the 10 years since the publication of the Institute of Medicine’s Crossing the Quality Chasm.9 But it is not yet truly mainstream because cultural change is slow, as evidenced by the equivocating commitment to patient-centered care in actual practice. Patient-centered care represents just such a systemic change requiring redesign of processes and socialization of values across nearly every function of institutional care. It involves:
• Inclusion of the cultural traditions of health seekers (patients).
• Personal values and preferences.
• Understanding and accommodating family situations.
• Recognition of personal lifestyles.
• Integration of health seekers and their families, close supporters, and caregivers with healthcare providers in making clinical decisions as an extended care team.
• Respectful, coordinated, efficient transitions between providers, departments, and healthcare settings.
User-centered design improves human interaction with technology, but does not challenge the logic of practice.
No clinician works from “anti-patient values.” But values conflicts show up in practice not as fundamental disagreements but as differences in method—in how things get done. Differences between clinicians and administration, doctors and nurses, and one unit and another are a source of conflict when each group has different preferences and priorities. Consistency and routine are maintained for coordination and safety purposes, and values differences are rarely examined. These stakeholders may not share a common values base, even if they serve the same explicit goals.
What are the unique values and roles served by design in co-creating care?
• How could human factors, UX, and service designers develop resources that connect to the culture and values of care and caregiving?
• Can we better contribute to healthcare transformation if design collaboration is treated as a care practice?
• Will design research be respected and included in decisions involving care delivery, based on a shared ethic and accountable contributions?
• Should informatics courses include a service and design track taught by design professors?
• How might we learn to create and design better clinical services as “attending” design professors?
There are many ways to express a caring design ethic, yet each discipline views their meaning of care differently. We can create a design practice of care—such a change in values is supportable and authentic. In design, several disciplines contribute to human and social care: inclusive or universal design, human factors design, empathic design, and human-centered design.
These fields share a common technical language of design and evaluation, methodologies, user behavior, and focus on the human use of and interaction with technology and systems. We are missing the recognition of care professionals, a shared language between professionals acknowledging the primacy of human care, and our own realization of a tacit values system now shared by physicians, nurses, and all clinical staff. These are not small gaps.
Care Design and Institutional Change
Organizational change programs, such as movement to patient-centered care, offer an opening for rethinking and redesigning other systems interacting with business processes. Yet when that opening arrives, the methods and experience bases of most designers/researchers may be unprepared for the complexity. Collaborating with domain experts and recruiting cross-functional teams are only starting points. Innovation projects engage larger, diverse groups of possibly disagreeing stakeholders to get to breakthroughs in understanding any complex situation.
Large-Scale Healthcare Innovation
The healthcare system is technically a “mess,” the pithy term used by Russell Ackoff to describe entangled, interconnected, wicked problems.10 Ackoff leveled the term mess at healthcare at a conference in 2004:
Study after study has shown that much of the need for the care that is provided is created by the care that is given; excess surgery, incorrect diagnoses, wrong drugs prescribed or administered, unnecessary tests. The fact is that the so-called health care system can survive only as long as there are people who are sick or disabled. Therefore, whatever the intent of its servers, the system can only assure its survival by creating and preserving illness and disability. We have a self-maintaining sickness- and disability-care system, not a health care system.11
The United States and other developed nations face a near-future crisis driven by the following well-known shared concerns:
• Demographics: Baby boomers are aging and living longer than any cohort in history.
• Health needs: Healthcare service demand is shifting from acute care to chronic and long-term care; at the same time, there is pressure to reduce costs across the system.
• Economics: The lack of common payer or universal coverage is forcing more people to use emergency and outpatient services.
• Industry: Competition is driving institutions to grow, absorb rivals, and differentiate by investing in new and expensive equipment.
• Organization: Healthcare staff face growing stress and work demand, and staff-to-patient ratios are declining.
• Medicine: Awareness and interest in patient-centered and family-centered care is increasing, while the number of primary care or family doctors is steadily decreasing.
In a “mess,” any isolated issue is connected to many others, all of which are symptoms of deeper causes, which themselves have evolved into new symptoms. Attempts to intervene in one problem (e.g., improving cancer diagnostics) may result in consequences that reinforce the mess (e.g., increasing and expensive false positives). Changing any process (e.g., to improve wait times for patients) without planning for a larger scale may create an exception for that problem that healthcare staff must work around. If clinical and communications processes are not redesigned to lead (not lag) IT deployment, the risk is high that IT vendor solutions—and their process values—will by default design the de facto clinical process.
Designing Inside the System
We are on the cusp of a major trend in systemic design in healthcare, based on the cost and management drivers for system-level change of organizations and practices. In lieu or in spite of national policy innovation, organizations will be forced into fundamental change of business and practice models that many are ill prepared to accomplish. Few consulting design firms and fewer institutions have the experience and method skills to accomplish the sociotechnical analysis, multidisciplinary design, and cross-organizational facilitation for these complex CD3.0 and CD4.0 projects.
A Case for Service Systems Design
Two schools of services design and management have developed recently: the design-led service design school and the scientific, whole-system approach of service systems.
Service systems science has become a leading methodology for systemic design in large-scale, high-complexity, high-risk service environments. Service systems are “dynamic value co-creation configurations of resources” connected through the fulfillment of value propositions with customers.12 Service systems fulfill consumer demands and provider requirements, coordinating people, organizations, shared information, and technology in a service-oriented business model. Services are designed as social systems.
Consider a complex service system example. The regional clinic has evolved into a “big box care” business model that is no longer sustainable. It reveals itself in the inflexible (nonreconfigurable) routines imposed by both administration and service areas. It is revealed in the siloed organizational structure that separates services by specialist profit center. In Chapter 6, one root cause of the primary care crisis (too few family physicians for societal demand) was found in an institutional business model that rewarded specialist care and not generalist medicine. In the meantime, increased patient loads in primary care were not mitigated by increasing equitable payments for the volume, leading to inevitable system-level inequities and bottlenecks in basic service. These service problems are consistent with the operating business model of hospitals.
Other cost factors contribute to the whole system. High-technology investments (new scanners, surgical suites, cancer treatment facilities) keep hospitals competitive by promoting their advantages in regional markets. Large medical centers consider such technology investments a preferred pathway to service innovation and a means of building market share. These investments shift costs and development to procedures and medical technology, creating the necessity to gain returns on investment for extremely expensive high-tech purchases.
Taking a systems view, this approach to “buying innovation” reveals a possible values conflict. Capital investments dominate budgeting and squeeze total funding, effectively limiting the capacity to support community-level care.
Systemic root causes are not yet business drivers in the health marketplace. Consider the impact of several causal trends on healthcare delivery: aging demographics, dramatically poorer health of families in poverty, increasing proportion of multiple chronic diseases, increasing population of large urban centers. All institutions are poorly prepared in general for these readily identified trends that will soon be root-cause drivers of future health crises.
A more effective innovation stance in healthcare services recognizes the need for top-down systemic redesign of institutional processes, practice and delivery, and business models. Bottom-up co-creation approaches (and what we normally call design thinking) does not intervene at the institutional scale, but co-creation methods are employed in the design of artifacts. Service redesign requires intentional organizational willpower to surmount the established mindset. Management sponsors and their protection during the research and design stages are essential for the project to survive the exploratory stages and inevitable criticism.
Iterative prototyping is not enough when the risks involve millions of dollars and human lives. Research on defined alternatives is required to build an evidence case for system-level change. To effect system change, a systems approach to research and design is needed. Solutions applicable to entire healthcare systems at the sectoral level can be envisioned by service systems design teams and assessed in iterative research processes (developmental evaluation13) or democratic stakeholder methods (dialogic design14).
Understanding Problems as Systems
Design and design thinking create artifacts and services that bring a preferred state into being. Designers proactively discover deficiencies and promote creative opportunities in hope of maximizing overall betterment. We are educated and rewarded to solve problems and help people resolve difficulties. But because of this, designers share a single bad habit—the compulsion to solve problems. We resolve those gaps between the way things are and the way things should be. High complexity requires the suspension of this cognitive style and helpful reflex. The combinatorial complexity of interacting social and clinical factors, unforeseen consequences, and emergent outcomes of healthcare require a systems thinking approach.
Every sector of the healthcare industry is riddled with problem systems with interconnected and insoluble situations. Because most designers do not have professional training in health sciences, we risk introducing unforeseeable errors and unexpected outcomes when pursuing conventional problem solving in highly complex interactions. Yet we are discouraged by institutional culture from using unconventional means of inquiry, design research, or generative design. Our clinical clients and users are educated in analytical methods and may have limited patience for discovery and collaborative design. We risk the appearance of “not knowing” in an environment where confident knowing is all important.
A Better Way to Problematize
Problems are “preframed” by members of organizations as they collectively attend to similar gaps and deficiencies. We can assume these problems often represent the effects of an unknown cause (e.g., an increase in medication errors) or data reflective of past history (e.g., clinic wait times). When we attempt to solve these “thin problems” as given, we underconceptualize their complexity and set ourselves up to, effectively, fix the symptom. By attempting to rapidly understand and simplify a situation, we are forced to ignore the complexity of systemic causes that may have interacted to produce these effects.
In a complex social system, analysis of its effects (e.g., acting on measures) is a path to slow failure, not resolution. If a problem is wicked, then traditional problem solving just wastes valuable time.
Traditional organizational and project management processes are poorly suited for complexity or innovation. Whenever we organize to fit the established steps of (1) problem definition, (2) analysis, (3) solution (or design), and (4) execution, an analytical deductive process is employed. In clinical situations, the problem definition is often based on a measured deficiency (e.g., emergency wait times) or a high-profile recognized need (e.g., EMRs). These are well-known shared processes for organizational action.
Systems thinking addresses the rationalizing bias as the central cause of problematic outcomes we attempt to address. In some sense, the ultimate root causes of individual, service, and organizational problems in healthcare are our own thinking processes and an unreflective reliance on scientific method.
A problem in clinical and scientific research is the reliance on a single epistemology, when multiple modes may be necessary to understand perspectives, dynamics, and consequences. Systems scientist West Churchman advanced a general theory of systems inquiry, being the process by which human knowledge is produced (e.g., research and design).15 Churchman mapped five eras of epistemology, or ways of knowing, and identified their modes of inquiry. Each frame has a signature philosophy and method, and each is legitimized—“guaranteed”—by a different type of evidence (Table 8.2).
TABLE 8.2 CHURCHMAN’S SYSTEMS INQUIRY
System of inquiry |
Guaranteed by |
Healthcare examples |
Empirical, inductive |
Consensus |
Social proof (e.g., checklist practices) |
Rational, analytic-deductive |
Logical consistency |
Evidence-based medicine |
Idealism, multiple realities |
Range of perspectives |
Patient-centered care |
Dialectic |
Conflict |
Policy making |
Pragmatic, systems inquiry |
Progress |
Service design, iterative practice |
Conventionally, these modes are in conflict, as different people in different settings disagree on what counts as legitimate evidence. A systems context considers them complementary methods for reasoning and research. Design thinking has no similar concept, but the Churchman modes might serve to integrate systems and design. For example, ethnographic research is based on inductive empirical observation, and its evidence and methods are misunderstood by those who require “hard” or quantitative evidence from experimental traditions or deductive hypotheses. In law, multiple realities are contested by the adversarial dialectic used to force a jury to a single claim on reality. Design research iterates over multiple observations and makes abductive connections between each sweep of the data.
The methods for “progress” require creative reasoning and mixed-methods research. In social sciences, methods are “triangulated” (combined) with complementary research to develop a stronger set of findings than produced by a single method. In a systems inquiry, methods are iterated progressively, allowing observers to learn from each session and review questions, methods, and participants as necessary. A progressive systems inquiry enables a research or design team to identify multiple, possibly conflicting causes and relationships in a problem, ensuring that the right problem and the best level of its complexity are pursued by the team’s limited resources.
Mapping Complexity in a Problem System
We can identify many sources of complexity in services and systems design. The most complex service problems are not those with inherently difficult content. Difficult clinical problems may have constraints that only allow certain approaches, and they can be treated as puzzles with a known best answer based on current evidence. Problems turn wicked when they live in the social realm. Stakeholders have varying goals and perspectives, incomplete knowledge, and insufficient collective understanding of the problem space.
Achieving consensus on socially complex problems requires we reach an understanding before attempting to design solutions. For multi-organizational and multistakeholder situations, that understanding should be co-constructed. Stakeholder management is a design problem, not an expert issue.
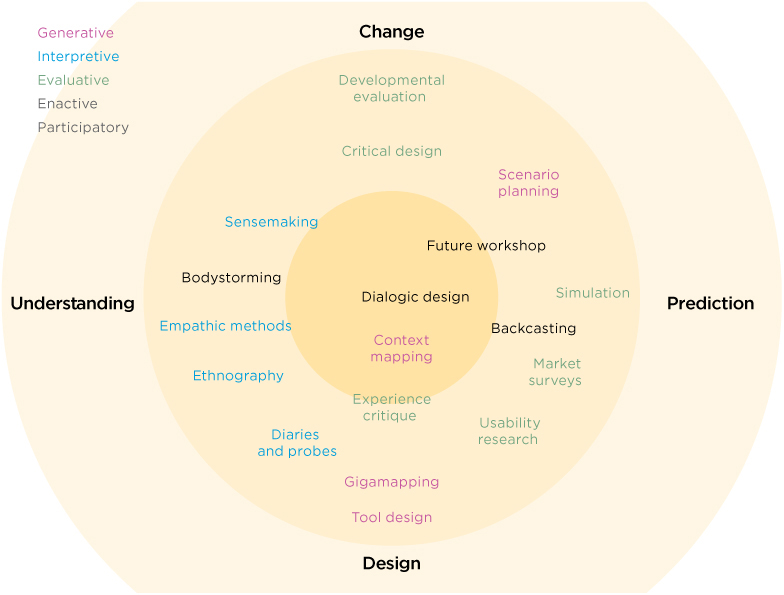
In such a case, we can choose generative design approaches and deliberative, structured design approaches. In high-reliability sociotechnical systems, using a generative design (co-creation) approach can significantly underconceptualize the problem, thereby coming up with interesting but essentially unworkable design concepts. The aesthetics of co-creative design workshops may not be congruent with the seriousness of the given problem in a medical environment. A range of appropriate design methods may be needed.
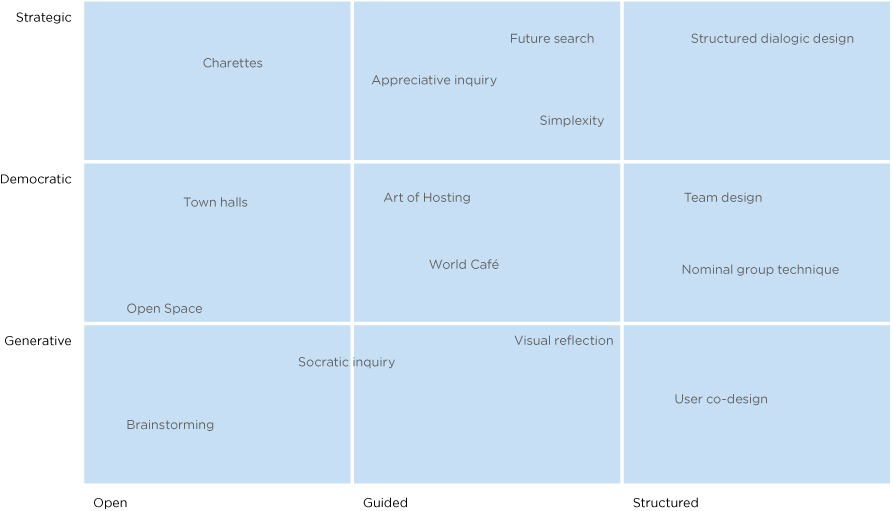
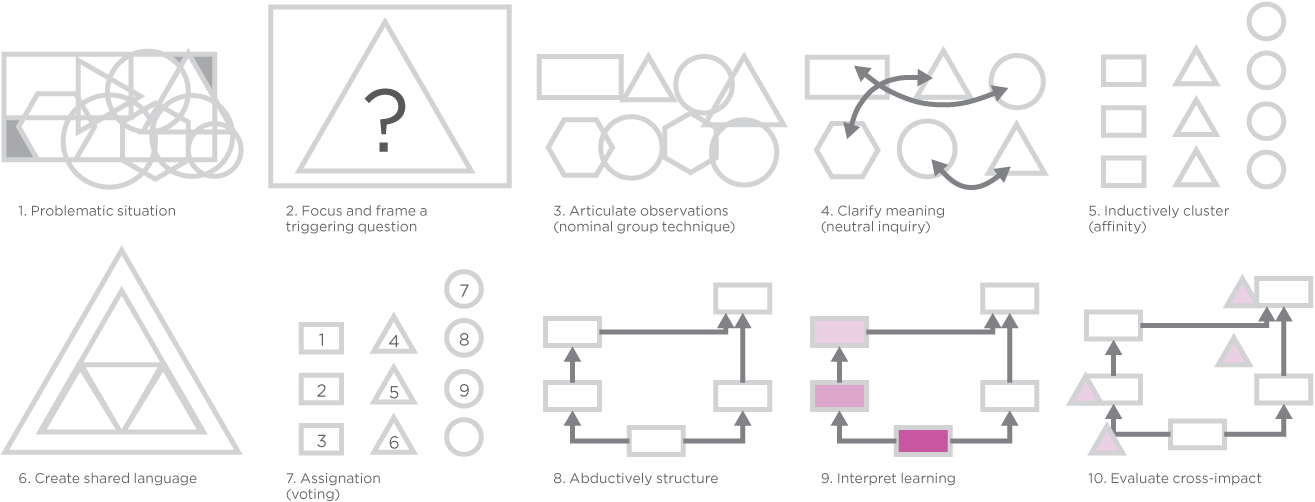
Strategic and structured dialogues provide a deliberative social design approach for complex services in serious domains such as medical procedure, practice organization, and service reconfiguration. Methods known as dialogic design provide a rigorous and engaging approach to elicit collective wisdom and collaborate on strategic solutions. In dialogic design, stakeholders are facilitated in group work to dive deeply into a shared inquiry, identify factors and systemic relationships, and then choose priorities and the best leverage among priorities.
Dialogic design produces a collaborative map of the problem system, or problematique, a systems model that reveals interdependent relationships in a diversity of perspectives. All of the viewpoints and priorities expressed in an inquiry can be considered and consensus reached.
The methodology has a deep history going back nearly 50 years. Wharton’s systems scientist Hasan Özbekhan developed the problematique as a framework for assessing relationships between overlapping and co-evolving problems. Özbekhan criticized conventional problem-solving approaches as antisystemic and ignorant of the cognitive basis of complexity: “We proceed from the belief that problems have ‘solutions’—although we may not necessarily discover these in the case of every problem we encounter. This peculiarity of our perception causes us to view difficulties as things that are clearly defined and discrete in themselves.”16
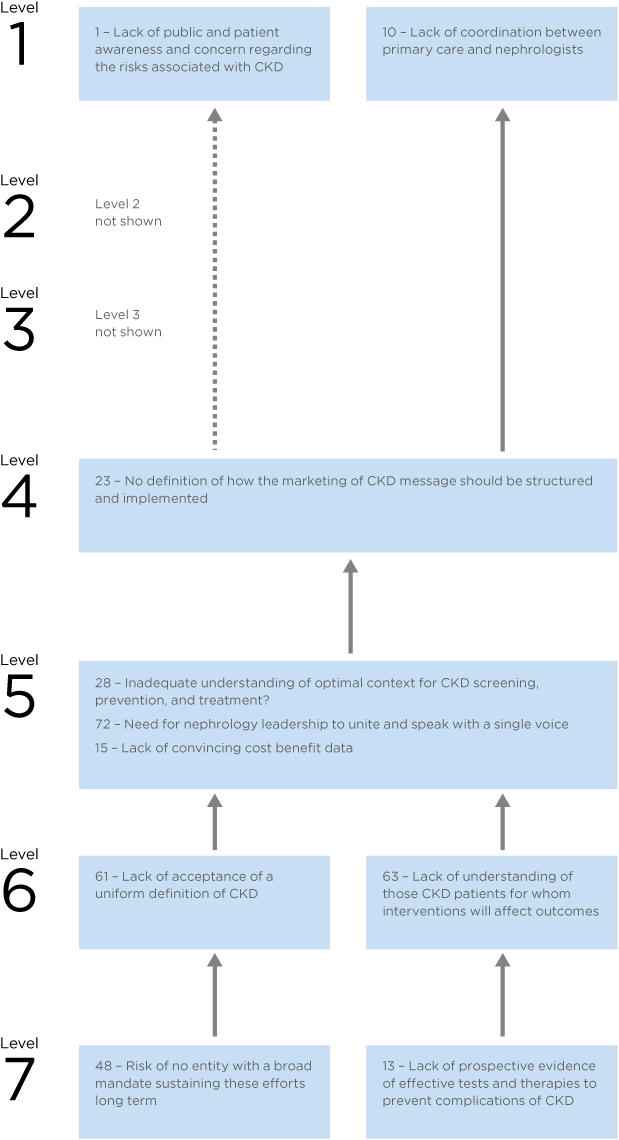
A problem system is mapped to reveal challenges and potentially high-leverage solution pathways in a map of problems structured by their mutual influence relationships. A published case study from the Chronic Kidney Disease Initiative sponsored by the American Society of Nephrology illustrates their problematique for the complex set of factors involved in chronic disease management (Figure 8.2).17 A workshop of 48 stakeholders representing 38 organizations engaged in structured dialogue to reach consensus on the problematique, using the Structured Dialogic Design (SDD) method (see the Methods section on page 288).
The SDD workshop facilitated consensus across a range of issues facing the 38 constituencies (of which only the consensus is shown in the problematique). The influence map is employed in strategic planning and group decision making, as it shows the agreement on foundational issues (at the bottom of the map) that influence all other issues (following the influence indicated by the arrows).
FIGURE 8.2
Partial problematique for the Chronic Kidney Disease Initiative.
As an action research and planning approach, SDD leads to organizational commitments to highly influential “root cause” actions. The map supports the resolution of issues with the most reach or leverage across the system. The goals of the Chronic Kidney Disease Initiative are common across healthcare:
• To understand the anticipated barriers that stakeholders will face in improving patient outcomes
• To build commitment to an action agenda to address these barriers systemically
• To forge a chain of partnerships that embrace the variety of stakeholders in implementing the agenda for improving patient outcomes
Stakeholders in the nephrology community generated the map in Figure 8.2 as one of several representations of dialogue constructed throughout the session. Participants engaged in a moderated workshop process that elicited individual responses to a framing question about barriers to action (problems). These “barriers” were transformed in several group language processes, using software (CogniScope II) to vote between issues to co-create this influence map. In this structuring of dialogue, root-level issues emerge in a consensus process and are recognized as those with the highest leverage to produce change in the system.
Issues at the top (level 1) represent the “most influenced” problems and are the visible effects. Barriers shown at the bottom (level 7) are the most causative or influential. The bottom two levels (6 and 7) tell us that (a) no group had a mandate to sustain efforts to improve patient outcomes, and groups acting independently would be unable to make progress; thus a systematic solution was necessary; and (b) physicians had no consensus on evidence for the relative effectiveness of therapies.
Some of the original factors were removed to better enhance the readability of the map. In the original, a single unconnected level I issue indicated the pervasive “worsening shortage of health care providers” as a major problematic effect. This is the same system-level issue known as the “primary care crisis.” It was disconnected because it was an independent outcome, and was not reinforced or influenced by any other problem in the map. It becomes a deep driver for the action plan, regardless of the chosen strategy.
The strategic planning outcomes were reported in a society journal to generate commitment across the specialty toward the initiative. Solutions were formulated in a second SDD workshop that mapped strategic design options—solutions to the “barriers” identified in the problematique.
System-Level Innovation
The chronic kidney disease case suggests the difficulty of effecting change at an institutional scale across organizations. In this model, clinicians (or any stakeholders) associated with organizations, regions, and subspecialties organize to accomplish agendas they have developed and socialized within their networks. Significant planning and a common determination are required to bring players to such a design and planning context. Yet when the system boundary is expanded beyond the organization, domain, or discipline—to achieve higher variety and broader impact—the difficulty of coordinating action increases.
Complexity increases when considering other chronic diseases that co-occur with kidney disease. If Type 2 diabetes and cardiovascular disease were included in the problem system (as occurs in the health seeker’s contexts), the root cause and barriers would expand beyond the specialist scenario.
The formation of mass opinion for a defined position has been necessary to motivate institutional change in the United States and Canada for the entire history of state-supported healthcare. Consensus building among competing stakeholders is a vital process necessary for changing business models and decision making at the systems level.
Today the enormous health sector has more in common with government and policy innovation than with business innovation. Simply implementing business-led innovation practices will not create a collaborative or innovative culture and has failed in institutional settings. The institutional values (of care) conflict with business (financial value) at a fundamental level. Design-led practices lend both cultures effective skills and means—D3.0 adapts well to organization and business contexts, and D4.0 methods to institutional and community contexts.
Changing System Behaviors
Systems thinking historically divides roughly into two major schools of thought: soft systems and hard systems methodologies. Soft systems includes social systems and dialogic design, and stakeholder-led processes. Soft systems have evolved from interpretive approaches, viewing social behaviors and purposive systems as outcomes of human agreement. Social systems may reflect actual organizations, but the systems are viewed as sociotechnical, cognitive, or languaging constructions.
Alternatively, hard systems are presented as engineering processes, with inputs, conditions, and feedback loops. Hard systems include system dynamics and cybernetics, including modeling and simulation—methods based on natural sciences and observable measures employed in information systems and living and ecological systems. Most hard systems methods define a clear system boundary and consider a system to be a real thing, an observable set of co-occurring behaviors “out there” in the world.
Both schools position the designer as leading “interventions” within a system as defined. For any type of system, an intervention is an action that disrupts system functions to enable a preferred shift of performance and behavior. The design role is to identify the range of options and choose the type of action, precise point of application, and timing of action or policy that creates a sustainable effect.
Systemic design as intervention is well accepted in the systems sciences. Perhaps the best formulation of leverage concepts is found in “Leverage Points: Places to Intervene in a System” by the late systems thinker Donella Meadows.18 Her “12 ways to change a system” still stands as an actionable and testable proposal for systems thinking approaches (Table 8.3). Their leverage is high because, if applied at the right point (and time) of force, the power of a single idea could reform an entire global system. However, these are the very ideas filtered and ignored by those maintaining the paradigm.
For example, John Thackara, a systemic designer who is not a physician, suggested that healthcare practice could become more like the system in Cuba, where 95% of the population is treated initially by family physicians located within neighborhoods.19 Care in Cuba and the United States is very different, as are socioeconomic conditions and resulting lifestyle diseases. Yet a distributed, low-intensity family care model has promise for rural and remote communities as well as large cities with dense neighborhoods. Today’s healthcare planning might screen out such proposals as infeasible or alien; yet such proposals may apply as well in developed countries.
Remarkably, Meadows’ formulation harmonizes across systems methods and removes some causes for disagreement. Hard systems modelers are able to identify leverage in their models and changing values, delays, flow rates, and so on. Social systems designers tend to focus on leverages 1–5, but have a meaningful checklist to map stakeholder ideas to their potential impact. This is a general, more functional approach to leverage than the barriers shown in the influence map (see Figure 8.2). The deepest barriers to patient outcomes in kidney disease were fundamental definitions and agreements that had leverage on everything else in the system. When determining solutions to those same barriers in the design stage, the understanding of leverage points would be very helpful indeed.
TABLE 8.3 LEVERAGE POINTS IN A SYSTEM
1. |
The power to transcend paradigms (e.g., patient-centered or evidence-based medicine) |
2. |
The mindset or paradigm out of which the system—its goals, structure, rules, delays—arises |
3. |
The goals of the system (e.g., efficient medical care or healthy communities) |
4. |
The power to add, change, evolve, or self-organize system structure (e.g., healthcare design roles) |
5. |
The rules of the system (e.g., incentives, constraints) |
6. |
The structure of information flows (who does and does not have access to information) |
7. |
The gain around driving positive feedback loops (e.g., reinforcing hand-washing practices) |
8. |
The strength of negative feedback loops, relative to the impacts they are trying to correct against |
9. |
The length of delays, relative to the rate of system change |
10. |
The structure of material stocks and flows (e.g., transport networks, population, age) |
11. |
Constants, parameters, numbers (e.g., taxes, subsidies, standards) |
12. |
Sizes of buffers and other stabilizing stocks relative to their flows (critical to concepts such as wait times for procedures or stocks of hospital beds) |
System Dynamics as Design Thinking
System dynamics encompasses a robust quantitative methodology for measuring the functions of a complex system and modeling their throughput and interactions. It is a popular approach in systems engineering, but not in design practice. However, key ideas in system dynamics can support design thinking and visual understanding of complex system behaviors. In healthcare services, care management, and policy outcomes, it helps to understand and illustrate patterns following the well-known language of system dynamics.
MIT’s Jay Forrester developed the system dynamics modeling approach as a way to formulate better decisions through prospective evidence for large-scale industrial and policy planning.20 Adapting the comprehensive WORLD model, Forrester identified ranges and assumptions to model behaviors of global population, industrial growth, energy consumption, food supply, and other trends. The simulation resulted in scenarios of unsustainable growth and resource collapse that were published in the best seller The Limits to Growth.21 When those scenarios failed to appear within a few short years, the exercise was debunked by business and growth advocates. Rejecting the move toward global stewardship, this sparked the unforeseen and unintended consequence of a generational culture shift toward consumption and away from precaution with respect to energy, environment, and global industrialization.
System dynamics has contributed prominently to healthcare research and to process design in hospital process and wait time studies. However, it remains unclear where systems thinking contributes to service or interaction design problems. For surprisingly complex design problems—for example, achieving adoption of hand-washing routines to reduce iatrogenic infections—we can plot expected behaviors against observed current states to elicit patterns to be mitigated.
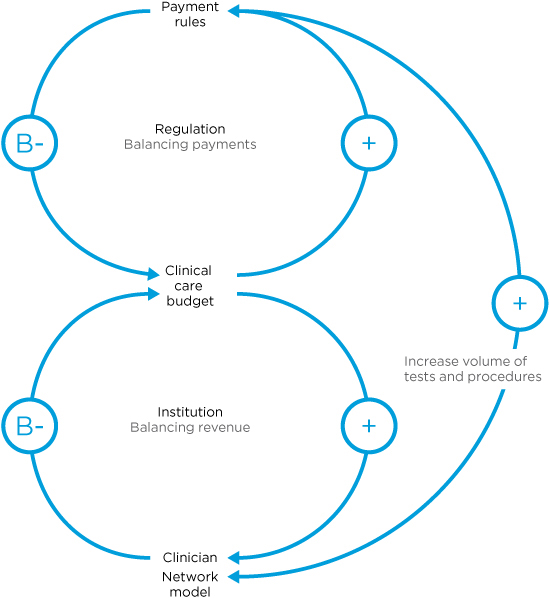
Systems have a purpose. Systemic behaviors repeat their operational functions on inputs to produce defined outputs. In so doing, they seek homeostasis (called “equilibrium” in mechanical systems). In social systems such as healthcare, homeostasis regulates a process to ensure that the human purposes of the system are met.
Human purposes have explicit goals (to provide health services) and implicit or tacit goals (to maximize profit from the payment system). The hidden goals are often the most powerful in systemic design problems because they are the source of the deficiencies we are trying to correct. They are especially powerful because we often cannot identify or discuss them directly.
First, consider the critical behaviors selected from a defined problem of interest. The functions are primarily based on stocks (measured supply of a material or state) and flows (inputs, outputs, exchange, and behavior). Often a simple stock-and-flow diagram is sketched to identify the basic mechanics of system operation. System dynamics excels at representing the forces of positive and negative feedback on system constituents.
Figure 8.3 shows a causal loop diagram, the signature visual representation of a system dynamics analysis. It is a sketch of the relationships between system components and their patterns of feedback. Causal loop sketches are portrayed by identifying commonly recurring problem patterns among the selected components to illustrate the dynamics of a complex situation.
A positive, or reinforcing, feedback loop is drawn as a curved line with a plus sign (+). It amplifies the flow associated with the arrow, or increases the gain in the component. It is not always an increasing (or “positive”) direction, as positive feedback loops can equally increase a destructive effect.
FIGURE 8.3
Causal loop diagram: “shifting the burden” archetype.
Negative feedback is shown as a balancing (B) loop and regulates the relationship between two things. A car’s cruise control is a classic negative feedback loop—it uses a continuous balancing loop to regulate power to maintain the desired speed setting.
The diagram represents a common system archetype called “shifting the burden.” Archetypes are recurring systemic patterns, the knowledge of which enables systems designers to quickly recognize dysfunctional patterns in a system. This pattern illustrates how physicians bypass the regulatory intent of managed procedure costs by increasing the number of related procedures as a workaround that maintains the expected income. Also called “over-treatment,” this function can be seen to have a systemic cause that has more to do with practice management than ethics.
Two balancing loops (associated with “regulation” and “institution”) each have a positive and negative loop, joined at “clinical care budget” (where the symptom appears). A third reinforcing (+) loop bypasses the symptomatic solution (payment rules) to shift the fundamental solution (managing physician revenue). This reveals the unintended consequence of regulation aimed at reducing healthcare costs across the system.
The “shifting the burden” archetype illustrates the problem with setting rational incentives as policy targets and expecting outcomes to match. Incentives have been identified as a recurring problem dynamic at the institutional level of healthcare, and like other “rules of the system,” are potent interventions. The trap of “perverse incentives” occurs when the unintended consequences of a defined incentive results in behavior precisely contrary to the intent of the incentive.
Another archetype called “success to the successful” is evident in the imbalance between primary and specialty care at the healthcare system level. A differential allocation of resources is positively reinforced for the “winner” and continues to draw from the “loser” (primary care). The United States spends roughly 5 times on physicians as its peers, such as Japan and the United Kingdom, which show equally good clinical outcomes and life expectancy. One analysis shows that the most significant driver is the much higher costs of specialists.22 Higher fees in the United States are driven largely by higher rates paid per procedure, and a larger proportion of higher-paying private (insurance) payers.
This is another design problem. The “success to successful” archetype is reinforced by the supply of residents in specialty medicine. The existing imbalance of specialists in US healthcare leads to poorly designed policy and distorted incentives. Society needs more primary care doctors, but there are no financial incentives to draw medical students toward this choice. Because subspecialists can outearn primary care providers on an immediate and lifelong basis, even idealistic medical students will choose the higher-paying career paths. Design at the level of policy could certainly help, by creating financial offsets for primary care, for example, or subsidizing school loans if residents choose to go into primary care. But the most difficult function in design is seeing execution through to making those decisions.
Reframing Design and Systems Methods
How does systems thinking help the designer in everyday practice? How can systems thinking be integrated with design thinking for improving healthcare services? Design and systems thinking are not integrated disciplines, despite many mashup attempts. They approach problem definition and problem solving in almost incompatible ways.
Systems thinking was developed over half a century of research, from systems theory, and applies scientific principles to social practices (healthcare services) and engineering problems (medical device design). The systems perspective is both holistic and analytical—by discovering whole-system behaviors and outcomes, human-centered design can be targeted to the sources of those effects.
This process is easier said than done—systemic design requires time up front to conduct the research, to unearth discoveries, or to organize stakeholders in the design process. Design projects are usually launched to target critical business cases, which may not even have an allocated research budget. Designers have to make the case for an integrated systems/design/research approach. Clinicians and clients need to be convinced on each case’s basis.
Designers have their own barriers to the process. We do not pitch or perform methods we do not understand. Systems methods may appear too structured to be considered “creative” practices and may even appear to inhibit the possibilities for design ideation. Improvisational design practices (design thinking techniques such as brainstorming or affinity mapping) are preferred by designers to structured systemic processes because of their agility—their ability to produce rapid results that are sufficient to the problem (as framed). The learning and planning costs are much higher for systems methods, and if their execution does not yield outstanding results, second chances may be harder to win.
Design thinking changes the game board when the rules of play cannot be touched. We can skip over the necessity to fully analyze problem structure and behavior by envisioning a different frame and outcome than the situation as given. In classical terms, this is called “reframing the brief.” Design researchers Bec Paton and Kees Dorst have shown how designers modify and negotiate the framing of design briefs.23 They describe an abductive reasoning process to identify new metaphors and a “better problem” to resolve than the issue as given. Although this process risks possible avoidance of the complex set of problems a healthcare client may present, the systemic inquiry process (which they term a “journey”) reduces the risk of expending resources solving symptoms and bringing superficial relief.
The reframing process is driven by three steps:
- Use of metaphor and analogy: reframing by adopting visual abstractions to rethink a situation
- Contextual engagement: inquiry with problem owners to deeply appreciate the context
- Conjecture: co-creating new ideas as “what if” scenarios
And reframing is inhibited by three barriers:
- Cognitive fixation: following the “garden path” of predetermined projects and ideas
- A problem-solving mental model of design: attempting to fix a deficiency as stated
- Resistance to the journey: unwillingness to explore variations over time
A team’s initial understanding of a concern or a “fuzzy situation” is always insufficient and is often biased by precedents, groupthink, or prior work. Design and health cultures are biased toward action and outcomes, and dialogue (inquiry) is discouraged when schedules are compressed and stakeholders hold an expectation of professionalism. We need good techniques to deftly slow the rush to action and sustain an inquiry.
The Third Thinking
Healthcare problems are known to be complex. They demand a combination of systemic and human-centered design methods. Yet in health practice (and in consumer sectors) wearing two thinking hats is not enough—we need a third hat of domain knowledge. A care service orientation requires thinking like a care professional, one with a holistic view of patients and their communities, healthcare practices, technology, and policy.
The designer role, while still a creative activity, leads by facilitation and co-creation with stakeholders in designing care service. They convene and lead circles of stakeholders, designers, care providers, and patients to collectively gain and visualize a deep understanding of complex issues.
The structure, organizational collaboration, and evidence are precisely why these methods are effective in healthcare. Organizational project management is not the best approach for wicked problems. We often have a single chance to plan or propose a new project, and winning proposals have to account for a complex range of decision holders. Internal stakeholders may include clinical services, administrators, business and finance, and marketing. External stakeholders can involve community advocacy groups, policy makers, regulators, corporate partners, and other community members and organizations. Not to mention the patients!
This level of complexity becomes unworkable with innovation practices that rely on the creative emergence of ideation. These stakeholders represent significant positions and histories in their communities, and they do not share common goals or outcomes. Collaborative governance and decision processes are not facilitated by creative brainstorming. Social systems design methods discussed in this chapter (such as SDD), and the Positive Deviance and Simplexity methods described in Chapter 6, have been integrated with design practices and rest on formidable bases of evidence. For high-risk, multistakeholder complexity, these industrial-strength methods can be engaged, at least within a spectrum of practices.
• Systemic design integrates services and IT systems to the entire organization and its ecosystem. Systemic design achieves design goals through D3.0 practices (within the organization) and across institutions and health ecosystems or within communities (D4.0).
• A primary goal of systemic design is to gain collective understanding about a problem system and to discover effective interventions based on shared wisdom. Design methods are used to create artifacts that bring scenarios, options, and leverage points to life within abstract system and behavioral models.
• Systemic design requires multiple sketches or views be made of the whole system. Methods of system mapping and life-cycle workflows visualize the processes, boundaries, and systemic relationships among actors and other systems.
• Experience and systemic design are complementary to each other. Systemic design maps services and IT interactions for a given area. Experience design maps the individual health-seeker life cycle to services and systems.
• A clinical service system is concerned with fulfilling care, the outcome of service. The design of processes and procedures are reconfigured to achieve human system goals.
• An organization’s business model reflects its values and operational principles. The business model is a top-down process model that can be redesigned for new collective goals. A sustainable business model can be designed to produce value in the clinic and the community as an integrated service system.
• Service systems touch a large number of stakeholders and require multiple socially oriented design methods such as moderated group processes and design workshops. These methods may be novel to stakeholders, and organizations should engage skilled design support when first learning and using these methods.
• Systems and design thinking methods are enhanced by consciously framing and reframing the problem as given or stated. Reframing is itself a design process and is improved by collaboration, sketching, and critiquing ideas.
Case Study: Mayo Mom Community Health Service
The following case was a proposal illustrating the direction of integrated service design. It offers a model for service innovation based on a deep appreciation of long-term business goals, health values, and community needs, and the systemic drivers that link these.
A team from OCAD University’s Strategic Foresight and Innovation program won the 2011 Rotman Design Challenge with a unique service design proposal to facilitate children’s health.24 Sponsored by the Mayo Clinic’s Center for Innovation, the concept employs an online social network to connect new and experienced mothers in both live and online communities.
The Mayo Mom concept leverages the understanding of deep drivers in a social system and enables motivators for learning and behavior change. Mayo Mom is designed to facilitate breastfeeding, one of the earliest life determinants of future health, and therefore a powerful preventive health practice. The US Surgeon General’s 2011 Call to Action to Support Breastfeeding provided framing and impetus.25 Breastfeeding is correlated with fewer infections and diseases, such as pneumonia, asthma, diabetes, and obesity. The United States has one of the lowest rates of breastfeeding of any country in the developed world (only 13% of children are exclusively breastfed for the first 6 months). If 90% of US babies were breastfed for their first 6 months, more than $13 billion per year could be saved in healthcare costs.
Mayo Mom helps new mothers adapt to the experience of breastfeeding as a pathway to preventive health for mother and child. It demonstrates how simple design methods, even in prototype form, can inspire the development of critical social system changes that improve health. By taking a systems view of the breastfeeding experience, it was possible to look outside the traditional boundaries of the healthcare system to design an intervention that could improve a first-time mother’s experience when it matters most. Helping to shift the perceived problem around breastfeeding from one of education and access to one of social and cultural breakdown, the design team ultimately reframed the role of the targeted service provider, the Mayo Clinic, to a facilitator of community health, rather than just a provider of care.
Preventive Health as a Service System
Preventive health is a classic wicked problem, as the right actions must be taken and ineffective actions not only waste time but allow a health problem to evolve further without a response. Preventing a disease from occurring later is “counterfactual” and impossible to measure within a person when it does not occur. (Prevention is measured across population samples.) Community-level prevention programs usually focus on social determinants (such as housing and education) and root causes (such as early childhood diet in obesity), while advising at-risk individuals when they show up in primary care. The results of investment in root causes may not register for years, and programs must maintain a consistent campaign for years to collect longitudinal data.
What unique contributions can service innovation make to the prevention of multiple diseases across a population? How does a healthcare design team decide the best level of investment for the fuzzy return?
The immediate and long-term benefits of breastfeeding are well documented, and the opportunity for Mayo was identified to help new mothers by establishing a distributed community of care. The design team started from a set of design principles to effectively design for prevention:
- Be human-centered.
- Intervene in key moments of wellness.
- Be focused, simple, and decentralized.
- Create personalized knowledge, not information.
- Start early (really early).
The service design team followed a design research strategy portrayed in Figure 8.4, adopting an exploratory approach (diverge) to formulate the right problem framing, and then using focusing methods (converge) to design for the best alternative solution. They engaged mothers and childcare experts in interviews on the experience of breastfeeding, exploring the root causes and sociocultural constraints that inhibit mothers from reaching that 6-month mark. Critical to the design process was the search for a “key moment of wellness.” Without finding a specific moment grounded in time, space, and deep emotional need, a systems intervention can remain too abstract, losing critical focus and sensitivity to its context.
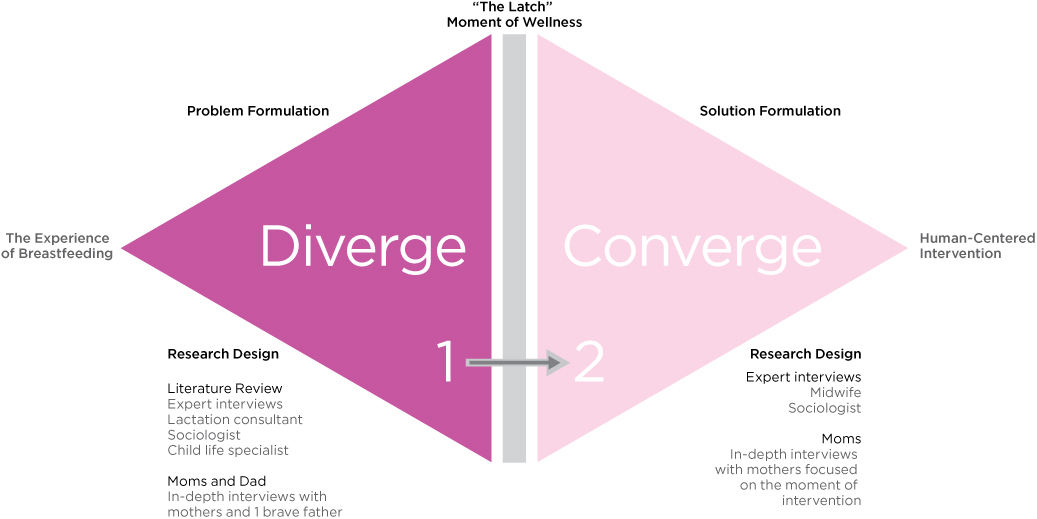
FIGURE 8.4
Service design research plan for Mayo Mom.
The initial “divergent” phase of the research process concluded in the identification of a specific moment called “the latch”—the critical period during a new mother’s breastfeeding experience in which she tries to establish her first connection with her baby. Success in this moment had a significant effect on a mother’s relationship with breastfeeding. This discovery gave designers clarity about where to “converge” and focus efforts to design a service system capable of improving her chances of success.
The research uncovered that US society’s aversion to the topic of breastfeeding creates a climate in which the deep physical and emotional challenges of achieving a good latch are not openly discussed, even among family and friends. Instead, a myth is perpetuated whereby new mothers are led to believe that a good latch will “come naturally.” Without disbanding this myth, the almost inevitable struggle of achieving a good latch can cause an otherwise confident and stable mother to doubt her own body, and even her ability to care for her child. Although not the only cause, this emotional turmoil creates enough personal doubt and feelings of failure to play a prominent role in a mother’s decision to turn to formula prematurely. This emotional experience remains pervasive among first-time mothers, despite the current healthcare support systems and educational programs in place, suggesting that because it is primarily a social problem, its resolution is beyond the scope of the existing healthcare system.
Designing a Sensitive System
Mayo Mom was designed to complement existing breastfeeding services by leveraging one of the most abundant resources across local communities: the wisdom of experienced mothers. The Mayo Mom concept is based on an accessible online network that connects experienced Mayo-certified mothers in the network with first-time mothers who hear of the program during their prenatal care. The network facilitates personalized and emotionally supportive one-to-one relationships during the stressful time leading up to and during breastfeeding, focusing mainly on the month before and the month after birth.
Mothers who volunteer for the program complete a simple online certification module before they are entered into the service’s database and matched with a new mother in the online network. An essential component of the service system design, the certification enables new mothers to trust their Mayo Mom and builds a community of practice between Mayo Clinic and the certified advisors.
Before birth, the Mayo Mom relationship helps prepare new mothers for the emotional and physical challenges of breastfeeding. After birth, the experienced mother is there to offer socially unconstrained (potentially anonymous) emotional support and positive reinforcement as the new mother seeks to create a good latch. Mayo Mom reframes the Mayo Clinic’s role from that of a primary provider of care to a key facilitator of the network and a beacon of credibility for the service. Mayo Mom shows the possibility of care services that extend the clinic into the community. After all, most illness and wellness experiences occur outside the walls of the traditional healthcare system, and this is where many solutions are to be found.
LESSONS LEARNED
• Health value is realized in the ability of people to participate in their work and communities. New sources of value for clinical institutions will be found in the regional community of health seekers and their caregivers.
• Most everyday health needs are localized in people’s homes and communities. For clinical service lines to expand their reach into the community, they will need to coordinate both social networks and place-based human networks.
• Creative approaches to new health services will be discovered in response to both declared needs and small-scale prototyping. First Lady Michelle Obama’s concern for breastfeeding brought social attention to an overlooked issue, creating an opportunity for a new service that might otherwise falter. On the other hand, such a novel service would require the safety net of multiple iterations of design and testing before its public announcement.
• Unhealthy circumstances reinforce disease processes that might originate from a person’s network. Healthy communities support restoration of individual health. Design for communities considers home conditions, friends and family circles, autonomy and mobility, neighborhood safety, and food supply.
Design Methods for Systems Innovation
Most healthcare service design projects embrace common goals—to improve the delivery of healthcare, sustainably maximize the value of available resources, and enhance the health-seeking experience for people. At the system level, different measures of effectiveness are needed beyond usability and patient experience satisfaction. The customer defines the quality of a user-centered approach. Stakeholder satisfaction in a complex service system accounts for quality, staff performance, process, and of course, health outcomes.
Services are designed to fulfill customer value over a cycle from request to fulfillment, a series defined in a service journey. A service journey involves a series of products or communications delivered at each touchpoint or engagement. Incremental products are delivered over time to customers or subscribers, with a user-centered design focus on touchpoints. The atrial fibrillation (AF) case in Chapter 5 contrasts the design for service level (AF communications) and system level (practice redesign for chronic AF patients).
Both service design and service systems methods bring real value to healthcare design, but they have different purposes and outcomes. Selection criteria for the right methods are not yet well defined. For service design practices, the practical research and design methods are based on experience from fields with a well-defined customer and setting (as in retail). There is a need for relevant service theory that indicates when and how to select methods from one context to apply in another.
As the health sector has become heavily invested in during the last decade, a highly competitive environment has resulted. Therefore we have insufficient sharing of project experience for effective comparison of methods, as many providers prohibit sharing of their work and practices.
The D1.0–4.0 geographies are one set of criteria for method selection based on complexity and scale. The association of design methods with research goals is another. Design and system research methods can be mapped to their purposes in a simple framework (originally proposed for selecting information research methods26). Figure 8.5 maps the types of design research methods for service and social design based on four primary (non-overlapping) purposes or research goals.
When planning service systems, several phases of research and design are typical. Each phase may have a different purpose, initially to understand activity and the environment (phase 1), to design and prototype options (phase 2), and then later to design for system change (phase 3).
FIGURE 8.5
Design research methods by purpose.
Research methods are rarely conducted once just for a single phase—they are repeated to build a deeper base of knowledge applicable to each purpose. In UX projects, research does not always progress from understanding to change. Pure understanding methods such as sensemaking and empathic design research are often employed early in a project to construct a shared model of human social behavior.
Ethnography is a primary method for understanding, yet is relevant for all research purposes in a service systems context. Ethnographic field research provides some predictive capacity for cultural trends, often with a further intention to create change (design or social action) based on understanding. On the prediction side, market surveys as well as expert analyses (task analysis and usability research) and foresight enable analytical assessment and some degree of prediction based on qualitative or mixed data.
Change research purposes are system-level. Dialogic design and social participatory methods connect a bridge of action from understanding to change. Research for service systems requires both system and user understanding, and connecting those insights to design and organizational change. Design-oriented methods specialize in defining artifacts or services, not primarily the goals of change.
Service design at the system level requires a holistic understanding of organizational goals, management and caregiving capacities, and patient/community touchpoints. Nearly all new services in healthcare are necessary for managing the increasing complexity of (mixed morbidity) patient conditions, changing demographics, and institutional pressures for cost reduction and IT and service integration. UX-only methods, such as ethnography, surveys, and prototyping, are too user-focused. Design of complex services should be guided from the beginning with multistakeholder change planning and process/service design.
Dialogue as Participatory Design
Participatory methods are foundation methods for complex social systems. Designers have limited medical expertise, and most services cut across organizational lines, so a cooperative design approach draws from across service lines and management levels. We cannot work alone—even small efficient study teams can generate idealized models that can ignore or hide reality. We need participatory cycles built in to the process.
Design practitioners have adapted participatory workshops into the entire spectrum of design projects, from ideation through design to delivery. We must meet to make meaning together. Participatory design requires deep transdisciplinary communication, written and pictorial expression, and argumentation.
Workshop methods focus group attention on co-creation for a defined shared outcome, requiring planned facilitation. This trend has inspired facilitated design based on convening nondirective ideation (Open Space, World Café) and more structured facilitated methods such as Appreciative Inquiry. Organizations are increasingly adopting participatory and co-creative practices in their innovation life cycles, involving stakeholders directly in the design of their services. Methodologies for co-creation for complex systems are necessary, beyond the capabilities of open generative approaches.
Figure 8.6 shows dialogic methods across the range of systemic design applications, by structure and scale. These range from open and generative (brainstorming and its variations) to structured and democratic.
Appropriate methods are selected by identifying required outcomes and the appropriate stage of engagement and style for the stakeholders and context. Different design outputs are created with each of these methods, and though they can be joined in sequences, the relationship of one method’s outputs to the inputs of another is largely understood by practitioner experience. Several of these methods are commonly adapted together to accomplish stakeholder design.
FIGURE 8.6
Mapping dialogic practices in design.
Each method in the map follows a different process, but a common design language can be drawn from their process logic. The design language of divergence > emergence > convergence (see Figure 6.7) expresses a fundamental sequence of social design process found in Appreciative Inquiry, SDD, and Simplexity.
Generative methods (e.g., brainstorming, visual reflection) tend to be wholly divergent. Simple dot voting helps groups “rapidly converge,” but group voting elicits well-known errors and biases that result in suboptimal decision making. The first bias is thinking that generative divergence is sufficient to develop the field of options for selection; a related error is insufficient understanding of the options for selection; finally, simple multivoting leads to people selecting desired outcomes as their priorities, which always result or emerge from deeper systemic causes. Reaching agreement on outcomes (such as cost reduction) is antisystemic. System solutions are located in the highly leveraged actions that relate intended actions to each other to yield those outcomes. Those ideas are usually not big vote-getters (a principle known as the erroneous priorities effect).
Dialogic Design
Dialogic design deals with the problem of sociotechnical complexity increasing beyond the capacity of experts and management. Rapid progress can be made when stakeholders can visualize their understanding of the relationships among shared concerns and solutions.
Dialogic design was structurally formed to require the democratic inclusion of the requisite variety of diverse stakeholders for both ethical and design reasons. It is a true dialogue process. Dialogue is viewed as a multistakeholder inquiry by systems thinkers, a method of group research inquiry or designing.
Unlike common facilitated methods such as Open Space (as used in “bar camp” and unconferences), World Café, or idea brainstorming, dialogic design directly enables the following:
• Large-group democratic decision making
• Policy design and decision conferences
• Complex (wicked) problem solving
• Complex business service design and business planning
• Strategic and long-horizon collaborative planning
• Portfolio allocation and business strategy
• Problem identification and root cause analysis
We can never achieve complete understanding of a complex domain. We can use democratic, well-structured dialogue to maximize the wisdom of individual observations toward a more complete understanding.
Structured Dialogic Design
Dialogic design was formulated to enable stakeholder groups to resolve communication and decision issues common in organizational and innovation management. Its primary method, SDD, is a collaborative design methodology composed of multiple techniques that are “structured” following defined language patterns to facilitate effective group planning, design, and decision making. SDD is usually coordinated as a workshop with associated group decision software (for mapping and voting), but its essential methods can be facilitated as entirely manual processes.
Dialogic design evolved from Interactive Management, developed by systems scientists Alexander Christakis27 and John Warfield28 as a scientifically grounded method for social systems design. The method is validated by 50 years of planning and operations research, 40 years of scientific research, and 30 years in practice. As defined by Christakis, dialogue is “the participation of observers engaged in creating meaning, wisdom, and action through communication and collaborative interaction.”29
SDD employs design principles for a facilitated method of dialogue for decision making for wicked problem assessment and solution and scenario creation. SDD is based on reaching strong consensus across stakeholders.
All collaborative processes require sufficient facilitator capacity. Although SDD requires a level of training to accomplish well, a collaborative design process can be considered as effective as its facilitation, a paradox of collaborative design that is rarely acknowledged.
In a typical workshop, a distinct series of questions and prompts are presented to participants, based on the underlying logic of the language patterns shown in Figure 8.7. To facilitate process usability, SDD’s complexity is kept intentionally hidden. It is consistent with ensuring clarity of each step and the sense of true dialogue created in the live session by these methods.
- Define the problematic situation: A problematic situation is articulated and framed by a core team.
- Focus and frame a triggering question: A focus question is carefully defined as both invitation and inquiry, capturing the essence of the situation shared by all envisioned participants.
- Articulate observations: Stakeholders generate responses to the triggering question. Ideas are refined into statements; labels are posted.
- Clarify meaning: Facilitated group dialogue ensures all responses are clarified to the satisfaction of the idea owner (stakeholder). A catalogue of the responses and clarifications is circulated for real-time review.
- Inductively cluster: After clarification, stakeholders vote on the ideas they believe should receive deeper consideration in the system design. These ideas are clustered based on exploration of similarities.
- Create shared language: The group reflects on the formation of their first consensus structure pattern. Dialogue is captured as verbatim text associated with each statement.
- Assignation: A group vote identifies the responses that will be included in structuring.
- Abductively structure: With software support (employing the interpretive structural modeling algorithm), stakeholders vote on all ideas selected. Voting establishes the influence network among selected ideas, showing the collective assessment of influence relationships.
- Interpret learning: The influence map is discussed in reflection for group learning and meaning creation.
- Evaluate cross-impact: When both the challenges (problematique) and the solutions are mapped, the relationships of solutions to specific items in the problematique are constructed.
FIGURE 8.7
Language patterns in Structured Dialogic Design.
Each phase of SDD involves a separate, documented step, but there is significant flexibility and control in tuning the design for a planned application. These are basic language patterns, and experienced design planners can choose different techniques applied to accomplish the purpose of each step.
SDD is convened as a highly engaging, disciplined dialogue involving every stakeholder’s voice and input. Figure 8.8 shows how printed and handwritten statements for language patterning are organized visually for tangible group presentation.

FIGURE 8.8
Group clustering and labeling. (Photo by Linda Blaasvær)
• Dialogic and participatory design methods share a common perspective on the necessity for democratic participation of all relevant stakeholders.
• Participant recruiting for good requisite variety (multifactorial diversity) is one of the most critical factors in successful systemic design.
• Mixed-method approaches are typical in systemic design and supporting research. Compatible methods are selected for the targeted purposes of each stage (understanding, design, change). However, dialogic and participatory methods might be employed productively to some extent in every stage for complex design projects.
• Generative participatory design workshops are not inherently good techniques for systemic design problems. Generative workshops (ideation, open process, prototyping) have no system methodology for reaching a collective understanding or identifying system patterns.
• Dialogic design is uniquely powerful for systemic design in complex problems. But unlike open methods such as Open Space or World Café, SDD requires a significant level of facilitator experience to do well.