CHAPTER 5
Patient-Centered Service Design
Elena’s Story: Health Self-Service
Elena returns home to check on Ben before going back to work. Dr. Martin’s office calls at 4:30 to report the lab results. Because she experienced only a “mild” faint, Elena did not get a full set of tests. Her bloodwork showed a borderline diabetes condition called prediabetes, with a fasting blood sugar level of 112 (mg sugar/per dl blood) and a glycosylated hemoglobin (A1c test) of 6%.
Her other scores are mixed, with an elevated blood pressure of 140/92 indicating hypertension, and a high TSH (thyroid-stimulating hormone) level of 6 suggesting hypothyroidism and an overworking pituitary. Dr. Martin asks her to monitor her blood pressure at home. The nurse contacts Elena’s pharmacy to order the thyroid medication and a home blood pressure cuff. Elena schedules a follow-up visit in 1 month.
At home, Elena turns to websites such as Mayo Clinic and WebMD, as well as patient and health forums such as eHealthForum.com, to find information on hypertension, thyroid conditions, metabolic syndrome, and diabetes. Having multiple minor conditions troubles her, and she doesn’t see a pattern. Discussions on the online communities help her understand how other people are coping with hypothyroid and what to expect of the medication. She finds wide-ranging ambiguity in interpreting the tests for thyroid conditions, but she also finds evidence from health social networks showing that people manage hypothyroid quite well with her medication.
Adding a few new health tasks to her daily routine is not a problem. As a caregiver, Elena has formed attentive daily habits while caring for her father and during the normal course of motherhood. She fills her prescription, takes her blood pressure daily, and as an outcome of her renewed attention to her health and symptoms, starts feeling better and more in control.![]()
Patient Experience in Health Service
Elena assumes the identity of a patient as she accesses her right to healthcare. She has a diagnosis, medication therapy, clinical goals, and set appointments. To herself, she is not a patient, but a person seeking better health. Yet only patients have rights and legal options in the institutional system. Patient is a legal designation. From this point forward, Elena will be treated as a patient under care by the physician’s office and by the hospital associated with her insurance policy in a health maintenance organization network.
A patient is not fully a true consumer or a “customer.” Elena is not a medical market participant and is unlikely to seek another physician at this point or in future. She is expected to pursue health goals in the context of a patient and has little autonomy as a result. She could seek other treatment, end current treatment, or not follow doctor’s orders, but the risks to her health and the associated risks of personal economics limit these choices. She and her physician have essentially entered a care relationship agreement. Dr. Martin is clinically responsible for Elena’s physical care while under treatment, and Elena is expected to adhere to medication schedules.
These role designations are not just persona distinctions. The role makes a difference in nearly every design decision. Patients have rights to records, responses, and official communications, and to make their care decisions in clinical situations. Unfortunately, in the United States, people who self-manage their care outside the medical system have few rights to the resources of a healthcare “system.” As people quickly discover, doctor’s visits are often priced higher for uninsured patients than for insured patients with the same diagnosis, as offices are bound by system rules.
Cost-benefit decisions are not based on patient experience but on efficiencies and service delivery requirements. Patient satisfaction may be a critical measured criterion, but patient experience is not (yet) measured and integrated with service delivery.
Drivers for Service Innovation
Healthcare innovation is constrained by two structural drivers: (1) managing the risks of clinical services delivery for all types of patients, and (2) managing internal and network costs, as health services are delivered by highly regulated, shared service systems. These constraints maintain a focus on incremental, sustaining innovations at best, as opposed to radical (service) innovation. Regional healthcare systems cannot be disruptive in such an operating environment. They are the institutions that new services seek to disrupt.
With regulated or insurance-driven pricing, institutions are incentivized to grow large enough to distribute costs across their system and to raise sufficient capital for specialists and equipment. Hospitals invest in state-of-the-art facilities to attract practitioners and increase community visibility. But these drivers do not necessarily have a direct impact on the quality of care. Every institution claims a high quality of care. Yet quality of care can refer to many different measures. The Agency for Healthcare Research and Quality certifies four standards. The Joint Commission certifies 14 quality measures in its standards for National Hospital Inpatient Quality. These are outcome measures that reflect many different inputs. The measure of innovation is not as simple in healthcare as in other service industries. Successful innovation in mobile telephony can be measured by market share and adoption, as well as customer delight. Successful innovation in healthcare might actually be measured by improvements in critical safety and cost measures, as well as patient satisfaction. But the contribution of innovation is one of many factors in a complex sociotechnical system.
Many large US institutions innovate by acquisition. Large hospitals have the luxury of investing in differentiating equipment and facilities, such as the million-dollar da Vinci laparoscopic surgery system for minimally invasive surgeries. In clinics, acquisitions provide a path for innovating at the scale of service provision, allowing an institution to capture leadership in a service area. Acquisitions are “tangible,” as are certain investments in health IT (HIT); electronic health records, patient portals, and customer-facing websites increase and enhance patient experience touchpoints.
Yet HIT, merely acquired and not effectively integrated with service, can backfire. Information and interfaces are integral parts of a sociotechnical system—the social system that organizes work and tools into a meaningful function in an organization. When technological systems are merely “installed” into complex operations, social practices change to adapt. If the systems are not integrated well, entire system installations can be rejected at great administrative cost. Health service design facilitates the effective synthesis of clinical practice and organizational routines with new technology to improve internal or customer-facing operations.
The concept of innovation is often introduced in the form of equipment, devices, and new medical techniques. The value of service innovation can be difficult for managers to quantify and visualize. Redesigning processes and practices to improve patient experience can be viewed as less tangible and harder to measure. Service-level innovations such as patient experience enhancements or even improved wayfinding are more difficult to quantify and justify using the standard metrics of cost accounting.
This leads us to patient experience. Healthcare systems have not had to innovate the provision of service as a competitive function because end customers (patients) have had little power of choice over hospitals or services in a referral-based care system. However, with US healthcare reform, patients will have more choice, and service innovation will become a significant driver. More recently, some hospitals have adopted a service design approach to the coordination of patients and care within the institution. More institutions are expressing interest in understanding and measuring factors of the patient experience.
In the United States, new organizational models such as the accountable care organization and patient-centered medical homes encourage providers to form sustainable and independent practices closer to their communities. Though these localized clinics may not be innovative at first, they have more incentive to create localized or personalized patient services for complex care. A decentralized organizational form enables an entirely new range of services. Providing a single patient concierge across specialty providers or creating cross-network care teams will be possible.
Improved organizational capacity is critical, as new roles will be integrated and perhaps led by service designers. Service innovation still requires clinical staff, IT, and project managers. But the processes and methods may be quite unfamiliar to clinicians and managers at first.
Making Healthcare Innovation Tangible
The right design can help heal. Architectural projects and physical environments are measurable, accountable as assets, and serve as focal points. Evidence-based architectural studies have demonstrated that simple design changes to buildings, rooms, and patient areas provide an immediate positive impact on patient health and family experience.
Clinical improvements may not be recognized by patients, even if care service is entirely patient focused. Medical environments are quite opaque. Patients receiving poor care or unnecessary but expensive procedures have a limited ability to compare. Respect for professionals keeps people from judging their own physicians negatively. In a recent case, investigators at St. Joseph’s Medical Center in Towson, Maryland, discovered that the hospital’s peer review process failed to uncover more than 150 unnecessary coronary stents implanted under direction of the chief of the cardiac catheterization unit. Even after more than 600 former patients of the cardiologist were notified of the problem, most patients tended to believe the physician had done nothing wrong, and many were convinced that the stent procedure had saved their lives. Although an objective review might suggest this case was a dangerous and unethical violation of good service, most of the patient customers did not recognize this, and many were unwilling to accept the truth. This case shows how healthcare services have become too complex for the patient to assess risk.
Patients face information asymmetry and cannot make free decisions about care alternatives. Patients are not expected to fully understand the different procedures that may be available for a treatment. Although statistical risks and possible outcomes can be explained to patients, clinics usually follow a standard set of procedures. Physicians may choose the techniques they know best and can perform reliably and safely. The design issue is to tangibly help patients get better, which involves a mix of directed activities. Physicians may advise qualitatively different treatments and tests, such as lifestyle remedies for sleep disorders instead of anti-insomnia drugs. The health outcomes of lifestyle changes depend entirely on health seeker choices, which places initiative on the patient. We would be too optimistic to think that people will self-manage effectively—most people need strong support, which is something we can design.
Personalized service will grow, funded at first by differential health plans. Personalizing clinical service means regular and personal communication, concierge-style management of referrals and tests, and personalized care approaches. Care plans and pathways for unique disease conditions may be supported by clear presentation and patient education. The case study in this chapter provides an example of tailoring care pathways to accommodate individual differences in complex care.
Good Care Is a Moral Issue
Healthcare is one of the largest service industries across the world’s economies, but unlike most services, health care is an essential resource of modern life. It is institutionalized and in most nations managed as a public service, both as a public good and a natural monopoly. Health seekers are patients and not “care consumers” because they cannot self-inform sufficiently to make informed decisions among alternatives.
Cognitive science has argued and won this point. Humans are biased and irrational when making significant decisions, even when fully informed with the facts. Prospect theory, Daniel Kahneman and Amos Tversky’s Nobel Prize–winning thesis, demonstrated how people consistently overweight the prospect of possible losses and undervalue potential gains in considering decision-making outcomes.1 Called loss aversion, the theory shows that the emotional significance of a life or death decision, and the immediacy of the decision, place consumers in a weak position with respect to economic decisions that concern their health. Patients are likely to overweight the risks and undervalue potential alternatives. Because physicians are bound by the duty of care to recommend the safest effective treatment, patients may not hear about alternatives. Reconciling loss aversion into service design is a balancing act that challenges our ability to design better patient experiences. If we lived in a world of free economic choice and information equality, health seekers would be capable and confident of choosing nonmedical health alternatives, whether complementary or radical.
From a service perspective, patients are unique customers in this regard—they are discouraged from asserting agency. Patients are by definition subject to doctors’ orders and are even more vulnerable to the market power of healthcare policy. When the means to deliver resources for health restoration are concentrated in commercial interests, the opportunity arises to exploit the dire need and motivation of patients. Physicians are expected to be trusted advocates for health seekers, and most by far are honest brokers. Yet physicians are targeted by commercial operators as spokespersons for new and profitable drugs or for tests and procedures that they have the singular power to order and potentially profit from.
The regulatory system and rules of engagement have been layered into existence by private providers and insurance regulations for more than 50 years. Makers of healthcare products are merely seeking return on investment as actors in a healthcare service market. At the national scale, however, selling biological human needs to benefit corporate interests creates an economic moral hazard. In more complicated health scenarios, a single patient may trigger payment events in every one of the many touchpoints in a health-seeking journey—for examinations, medications, tests, and procedures. Today it is only too easy to monetize each touchpoint.
Advocates for caring healthcare services find the entire private healthcare system model to be unavoidably unethical, as the goals of the service providers and their end customers are permanently in structural opposition. Individuals are unable to change the system or even their role; they can only choose to remain in the healthcare system or leave it.
A Systemic Design of Health Service
There is no single service line of business in healthcare, no true end-to-end service provision. Unlike in other service sectors, such as banking or travel, the customer–provider relationship is multistage and diffuse. Its customers have a special legal relationship as patients, a designation that enables access to multiple encounters within a system of services. There may be no end point of service fulfillment, because managing health is an iterative and ongoing process. The value proposition of medical care is the most compelling offer on the planet: Every human being seeks health. And human health is uniquely manifested in every person’s experience and history, due to personal practice, history, environment, genetics, and interaction with infectious or viral agents.
The healthcare industry is widely diffused across business, government, and social sectors in the United States and Canada. An infinite expanse of touchpoints and interfaces can be identified or created for services innovation and improved design across the providers and networks for the different needs of care. For business and social service innovation, the opportunities are indeed endless. Yet these conditions also prevent innovations from scaling widely. There are no natural national populations of consumer service in healthcare, even in national healthcare systems such as Great Britain’s National Health Service (NHS). Different age and social groups have very different needs, and not all health needs are served in the same way or equally across geographies and societies.
Public healthcare (e.g., the NHS and each Canadian province system) may enable more opportunities for systemic innovation than the sprawling network of providers and payers in privatized systems. Systemic institutional innovation has high social and commercial impact, as changes to processes can theoretically affect any patient and provider. A technological innovation may only impact its clinical users and the types of patients that benefit from its application.
In the loosely coupled private system, investments in institutional innovation will only pay off for the hospital or system. Among a growing number of other critical expenses to consider, service innovation experiments are difficult to justify, even in terms of patient experience. Patients do not have the explicit choice of selecting an inpatient care facility; their physicians and coverage determine their affiliated clinic.
In a publicly supported system, however, an effective service advance can be trialed and validated, migrated to other institutions, and scaled to the regional or national level. One popular service improvement is reducing wait times in emergency rooms or special clinics (e.g., dialysis treatment). Although these service experiments are also sponsored by and conducted at single institutions, in public systems there are no competitive barriers to the diffusion of effective practice innovations to other locations.
Public funding not only maintains a single regulation control for costs and quality, but establishes a common client and funding source for research and system improvements. Healthcare service innovations from other countries and systems, where public costs must be saved, have assessed and published solutions to many common problems, such as wait times and care pathways. However, innovations do not pass between systems well; they are often restricted or at least not promoted outside the system.
Sociotechnical Services
Healthcare service redesign is an institutional-level process, which affords some possibilities for change but limits many others. Institutions change slowly, and organizations within them tend to maintain routines until they are proven less effective than alternatives. Work practices coordinating professional care are complex, and knowledge becomes embedded in practice, which is not easily changed. IT is slowly adopted, and rapid or agile practices are not yet integrated into most institutional IT practices.
Designers have to become part of the system to effect lasting change. There will be a growing need for integrated services design as the new healthcare organization forms build out. Architects and planners are today’s default design principals, but in the new organizations much more attention will be needed in organizational design, IT integration, and patient and community services. An entirely new type of design leader is called for.
These complex practices and institutions may require us to develop a different methodology for service design. Though we may treat healthcare as a service sector, the practices are sociotechnical systems, as found in education, energy, and security. The sociotechnical system is a social sciences perspective recognizing the interdependent organization of work practices, roles, tools, and technology. The goal of a sociotechnical system design is to integrate “the social requirements of people doing the work with the technical requirements needed to keep the work systems viable with regard to their environments.”2 As a whole social system, partial process solutions or policies can upset the optimal workflow established over time. Healthcare research and cases are rife with stories of disastrous IT installations that fail due to organizational practices and not usability.
Sociotechnical systems offer a research approach to the complex challenge of service redesign. Healthcare practices are seeking to integrate digital technologies and health records systems, and reduce cost overhead while providing better care to larger communities. Many so-called transformation programs have failed in the last decade because of the predictable systemic effects of social practices overcoming the best hopes of new technology or policy changes. In institutional healthcare (if not the consumer world), the service system is a sociotechnical system. Design proposals are supported and integrated by planned research cycles.
Sociotechnical systems in healthcare are organized at the topmost level by the common service delivery model of three clinical systems (in North America): inpatient, outpatient, and emergency. These are further organized by the functions provided by different clinical units or wards. Table 5.1 lists representative structures for three institutional types.
TABLE 5.1 THREE INSTITUTIONAL TYPES
Hospital |
Hospital/office |
Specialized center |
Inpatient |
Ambulatory/outpatient |
Emergency; special; long-term |
Acute and critical care |
Examinations and tests |
Long-term care facilities |
Intensive care units |
Chronic care |
Ambulatory care |
Elective surgery |
Simple procedures |
Pediatric care |
Emergency |
Outpatient surgery |
Neighborhood clinics |
Harvard professor and physician Richard Bohmer describes two basic healthcare “operating systems” that drive service and facility design models: the sequential and the iterative systems.3 These models can be seen as the end points of a spectrum instead of two distinct operational models.
Two different sets of service conditions are organized: sequential, for efficiently delivering standard care services to a large volume of patients; and iterative, when an ideal care pathway may not be known for the condition or patient. The essential structural differences are listed in Table 5.2.
TABLE 5.2 SEQUENTIAL AND ITERATIVE SERVICES
Sequential |
Iterative |
|
Mission |
Efficient delivery of known solution |
Evaluation and management of complex care for difficult problems |
Beliefs and values |
An ideal exists |
Ideal state is unknowable |
Scope of service |
Narrow |
Diversified |
Processes |
Standardized |
Nonstandard, or no protocols |
Management policy |
Centralized |
Decentralized |
Human resources |
Conforming, conservative employees |
Problem-solving experimenters |
Technology |
Specialized |
General purpose |
Adapted from R. M. J. Bohmer. (2009). Designing care: Aligning the nature and management of health care. Boston: Harvard Business Press.
The primary guideline is between the assembly-line efficiencies of routine care and “job shop” iterative processes for complex situations. Both of these modes call for different innovation models—incremental for sequential and exploratory for iterative. Sequential healthcare services can be improved incrementally, not radically, minimizing the risk in introducing variation to established organizational routines.
However, iterative healthcare is necessary for complex, multicondition, and unusual situations. Complex care requires multidisciplinary medical attention, rapid exploration and research, hypothesis testing, sensemaking, and multiple evaluations. If these activities seem to be defined as design process steps, this may reflect the underlying function of design and complex healthcare as logical problem-solving processes. In the same way that the scientific method supports deductive experimentation, the design process enables iterative problem solving with mixed reasoning strategies.
Due to the risks of coordination of procedures and communications, care innovations are designed as incremental innovations or changes within a well-understood sociotechnical system. Incremental innovation is not a bad thing. The goal of designing for care, especially in routine care, is to promote better health outcomes, not to improve business performance. Cost management is important, but managing complex patient care with safety and reliability is still the purpose, not creating new economic value.
Care Service Models
A practice can be designed to support a range of service types along the continuum from sequential to iterative, yet few facilities manage all types equally well. These service bundles represent different business models, as different value propositions are provided (primary purposes), and allocations of clinician roles, time, and shared services are needed for each variation. Cost and efficiency trade-offs must be made when integrating several models of care into the same facility, possibly with compromises in quality that would be unnoticed by patients. Simple examples of these types are shown in Table 5.3.
TABLE 5.3 MODES OF CARE IN THE SEQUENTIAL-ITERATIVE SPECTRUM
Sequential |
Sequential plus follow-up |
Continuous |
Iterative |
|
Primary purposes |
Screening |
Single disease |
Multiple chronic diseases |
Complex diseases |
Care mode examples |
Flu shots |
Type 2 diabetes with multiple therapies |
Congestive heart failure, diabetes |
Complex cancers |
System mode |
Primary care office |
In-store clinic |
Primary care |
Academic center |
Service design focus |
Communications enhancement |
Workflow and productivity |
Treatment flow |
Personalized problem solving |
Four service design approaches (bottom row) match the different mix of iterative/sequential care modalities. For sequential care such as public health outreach (flu shots) and conventional office visits, enhancing communications and access to care are typical design options.
Redesigning the provision of service is done incrementally. Service in the sequential care modes can be enhanced by direct design improvements, ranging from staff and patient workflow to specialized IT resources such as local electronic medical records and dictation transcription.
Continuous and iterative care demand a multidisciplinary innovation approach consistent with sociotechnical systems. Costs and errors increase with the complexity of multiple disease conditions and complications. Productive innovation opportunities are found in evaluating effective care pathways for complex care. Clinical care pathways are management guidelines for patient care for predictable, multidisciplinary clinical encounters wherein interventions are well defined and sequenced.
Care pathways are preferred organizational processes for care service, represented as flowcharts or decision trees indicating the different conditions, measures, referrals, and clinical choices available in a given disease scenario. These pathway models, or “algorithms,” describe a preferred methodology for case services for a known disease condition. The most advanced example of a care pathway system is the Map of Medicine (www.mapofmedicine.com), currently used by NHS providers as a service redesign support tool. These maps are proprietary, but a representation of a common pathway application is depicted in Figure 5.1.
Customized and iterative care is expensive to carry out and difficult to justify in many institutions with factory health business models. Custom care pathways may require full-time, flexible professional staff not assigned to other services, and well-coordinated practices for optimizing patient situations and rapid clinical problem solving. Consider Elena’s care pathway, which is unfolding as a conventional cardiac arrhythmia situation. But if her thyroid condition worsens and her metabolic syndrome intensifies into Type 2 diabetes, the convergence of multiple chronic conditions would escalate her risk, and these three (or more) disease processes would have interacting consequences. Without her taking personal agency to improve her well-being, her multiple conditions would trigger a customized care plan and specialized care team treatment.
These are not workflow situations but complex human system problems. Iterative care may require consults with specialists and multiple tests, running a risk of multiple interpretations and treatment trials. Practitioners also have access to specialized resources to help guide decisions. But the interaction of conditions requires research beyond the canonical cases, where expert intuition and experience make all the difference in decision making. As the developed world’s population ages, cases of multiple chronic illnesses will become more common. To deal with the sheer volume, society will invest in a better approach—a sociotechnical services design.
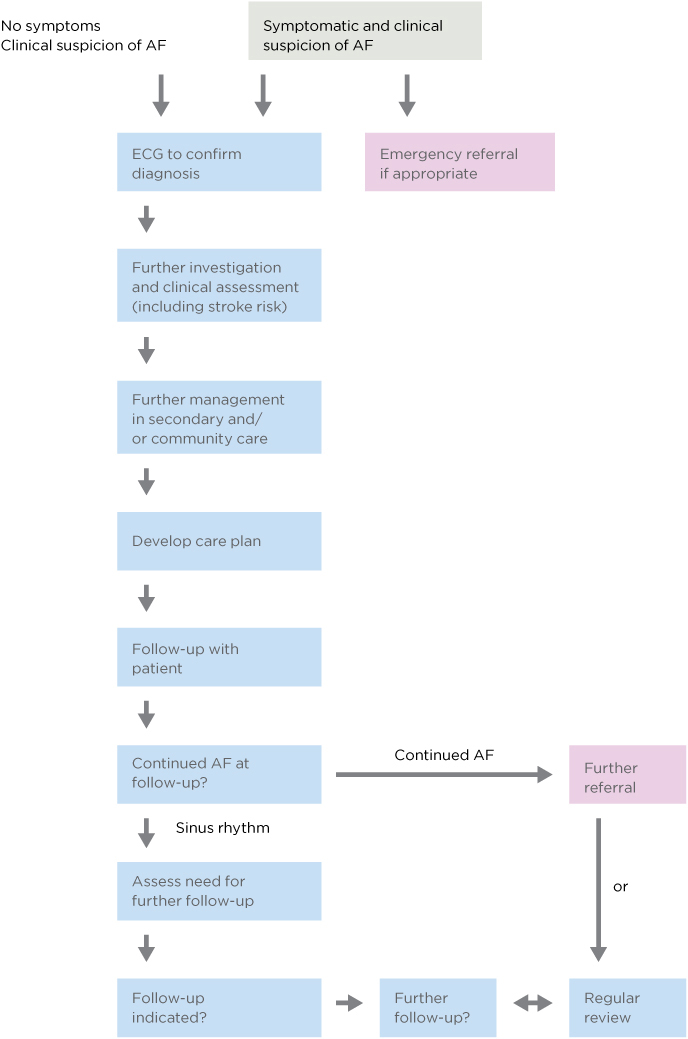
FIGURE 5.1
Care pathway for atrial fibrillation (AF).
Care delivery is not yet designed as a service offering, and there are no design practices yet for healthcare service systems. Care processes are first designed as clinical protocols, “designed” by specialized multidisciplinary clinician teams in committee processes. Clinical data tools and artifacts such as nursing shift change documentation, care plans, procedure protocols and checklists, patient data, and interview questionnaires are created by senior interprofessional teams, but without the benefit of visual design or sensemaking support.
There are significant opportunities for design thinking in this critical care process. Designers want to see iterative changes in the designed environment to sustain ideation and refine systems based on use feedback. Yet even so, prototyping and visualizing nonmedical services is quite simple compared with mapping clinical care pathways and medical decisions in a hospital or health system. Designers must acquire a much deeper level of domain knowledge to be effective than is expected in other service areas.
Evidence-Based Service Design
Inpatients spend most of their time during hospital treatment and recovery in a bed, often in a shared room. It might be obvious to anyone who has visited a hospital room that the experience of resting and waiting in this sterile, artificial environment could be greatly improved. The everyday experience of the inpatient constitutes encounters with the physical environment—from building architecture to room layout and furniture—and the presentation of services within a hospital and specialized clinics. Most of these environments leave a lot to be desired, and designed.
What if it could be proven that people heal demonstrably faster and better in beautiful, well cared for physical environments? Architecture professor Roger Ulrich’s research into the direct beneficial health effects of natural and harmonious surroundings during care provides hard evidence to support this theory.
Ulrich’s 1984 article “View through a Window May Influence Recovery from Surgery” was the first scientific recognition of the capacity of nature to accelerate healing in the clinical environment.4 Taking a patient-centric perspective, Ulrich demonstrated that natural scenes and emotionally supportive artwork facilitate significantly faster recovery and shorter hospital stays. Living plants and natural scenery produced the best results. Artwork content, not quality, makes an empirical difference. Scenes of nature, placid landscapes, and animals measurably quickened the healing process.
Ulrich also formulated the theory of supportive design, proposing that healthcare environments can improve outcomes directly by promoting stress reduction, buffering, and coping.5 Chronic stress severely limits the rate of recovery and delays the release of patients in acute and critical care. Supportive design focuses on the physical and interactive characteristics of the hospital to reduce the occurrence or impact of stressors such as intrusions, constant noise, loud or unwanted sounds, and cluttered or sterile visual fields. There are a multitude of passive service touchpoints for increasing comfort, ease, and even intimacy. The conventional models of systems workflow in service processes can be detailed to show anticipated patient sensitivity and responses to touchpoints (both figurative and literal points).
Evidence for Design
Ulrich’s research originated evidence-based design (EBD) in the early 1980s, which started in hospital architecture and expanded to care processes, practice interventions, and device design. As in evidence-based medicine, the current “best evidence” in literature and practice is recruited to support decision making, with the explicit goal of optimizing defined health outcomes in measurable terms.
Evidence-based medicine relies on the highest appropriate standard of evidence for a clinical decision. The cultural and regulatory adoption of evidence-based medicine has created an environment of risk reduction that demands a similar clinical standard of evidence for any research-based decision, including IT or services. For well-known diseases, the randomized clinical trial (with blind control and experimental conditions) represents the “gold standard” of evidence. Needless to say, that standard does not apply in design research. But it conditions the culture in which design decisions are made.
What is the appropriate level of research rigor for design decisions for health? A major goal of EBD is to ensure research is transparent and repli-cable, so that other institutions can learn from the study. A secondary aim is that of communicating the effectiveness of service design and research methodologies through institutional research, demonstrating validity and appropriate applications in the professional literature.
The interface of a health records system could be measured not only through formative usability testing but for its actual performance in clinical service. Progressive hospitals with strong informatics departments, such as the Children’s Hospital of Philadelphia, measure and track patient outcomes as a hard metric to determine the degree to which defined health measures are improved by their IT investment. If design research methods remain proprietary or applied only as commercial engagements, the value of design-led research will not be fulfilled on a wider scale.
EBD is not just the gathering of user research to inform design decisions, as in a user-centered design process. It is a rigorous equivalent to the careful application of scholarly evidence in informing care decisions, and generally includes the following activities:
• Reviewing current and retrospective research to identify precedents, mature findings, and prescriptive guidance from relevant studies
• Prioritizing and balancing the literature basis with primary data collected from actual patient data, subject matter experts, and professional observations
• Advancing theories and hypotheses to support observations, and structuring evaluations to test outcomes of design decisions
• Measuring outcomes after implementation, and assessing theory validity and any gap between observations and hypotheses
What Evidence Counts in User Experience?
Few design disciplines face the risk position of architecture and device design in health institutions. Devices must be approved by US Food and Drug Administration review committees, and architects certify their designs and are responsible for the plans followed by builders. Software user interfaces designed for standard operating systems are not subject to equivalent certification. Does it make sense for UX design to adopt evidence-based principles in healthcare?
Design trade publications and UX blogs show growing interest in EBD. The typical claims made for evidence (largely qualitative) do not build credibility when evidence is merely based on user observations. Usability testing is an essential evaluation method, and is especially useful when applied across the installation life cycle of HIT.6 Yet usability testing cannot measure health outcomes, only user inputs and responses to interactive systems. In a sociotechnical context, it is supplemental but not sufficient evidence. The quality of evidence for assessing interaction design relies on the behavioral measures of task completion, error rates, and time on task. User satisfaction and, occasionally, learning rate measures are collected as evidence for design decision making. Yet no websites make the claim of improving one’s life and health following the interaction.
Through iterative research on prototyped sociotechnical systems, better design can demonstrate outcomes based on measures of patient health. Measuring outcomes in response to service change requires longitudinal tracking of patients across cohorts large enough to measure an aggregate difference. This is unlike any process in Web or interaction design. It suggests a gap in health service design research methods. When lives, liability, and dollars are at risk, the due diligence of quantified evidence is necessary to ensure decisions are supportable across the organization.
Evidence for Design Outcomes
In medical practice, scholarship, care planning, and design decisions, “evidence” differs significantly—not only the types of evidence, but its definition and collection, quality evaluation, controls, presentation, and publication. For clinical decision making, typically accepted evidence ranges from randomized controlled trials (gold standard) to expert studies (weak), including a variety of types of evidence (observations, imaging, measured variables) relevant to diseases, biological responses, and applications to procedures, interventions, and public health.
Traditional operational studies rely on “outcome measures,” but the measures taken often assume a causality between interventions and outcomes—a causality that may not always exist in a complex reality. Some clinics invest heavily in biostatistics research to infer outcomes associated with interventions, a complex but increasingly necessary undertaking. Evidence by type—from more to less rigorous—might include:
- Controlled human interaction experiments; mixed-method studies (triangulated methods).
- Patient observations; physiological measures; field experiment data (strong empirical).
- Robust sampled ethnographic data; controlled usability interaction studies (empirical).
- Small sample interviews; “hard” (rigorous, evidence-based) case study; extrapolations from field research.
- Expert opinion; heuristic or multiperspective assessment.
With the growth of the Web and the number of people needed to build it, the UX field has expanded well beyond the original human factors community that started the field. The widespread adoption of “user experience” glossed over many of the original distinctive differences between practices. Although this merger has gained a broader acceptance of the practice, this general acceptance is less relevant in high-hazard, high-reliability settings. Today research professionals constitute an ever-shrinking proportion of the field. A different “standard of care” is necessary when designing a system for clinical professionals or patients rather than for consumers.
EBD established a rigorous research methodology for healthcare applications understood in principle by practitioners. But not every informatics user interface or health website requires strong EBD validation. An insistence on EBD standards in the early stages of a design program could significantly inhibit the innovation value from exploratory research. Allow formative design and organizational learning to at least reach a stage of development where summative evaluation on prototypes and service concepts makes sense.
Service Design for Care
Is the healthcare industry a pure service sector? Nearly every interaction—direct care, informatics, insurance processes—is part of a larger service system. Even clinical devices, ranging from medication infusion pumps to MRI scanners, exist within a high-touch service system with standard procedures. To be adopted or even meaningful, HIT innovations require integration into the context of a service system.
Almost any durable device or medical product is part of a procedure that delivers the product’s value as a clinical or patient service. Every touchpoint in a clinical encounter represents a direct human service or a “surrogate” service. Hospital rooms, communications, nursing, treatment, even billing are services that can be improved by better design. Medications are not merely delivered to pharmacists and hospitals for patient use; they are highly staged services within an entire pharmaceutical industry ecosystem, physician understanding, and a prescription system.
Devices, medications, and even informatics systems attempt to disrupt service as minimally as possible in order to enhance adoption and minimize training, usage error, and liability. Changing routines in healthcare is not a trivial matter. The problem is not so much one of institutional barriers to improvement as it is one of committing a complex organization to a procedural change that risks new errors incurred by communication and coordination issues.
A Service Design Methodology for Healthcare
Can a service design methodology help clinical teams glue together fragmented experiences for a better healthcare experience? Design theorists John Rheinfrank and Shelley Evenson articulated how services were becoming experiences, and that design would evolve toward the flow of service experience. The aim of design for service was seen as “moving from ‘user-centered’ design of things to ‘ability-centered’ co-construction of meaningful experiences.”7 The foretold shift from a service to an experience economy will eventually inspire changes in healthcare. Children’s hospitals are perhaps the current leaders in “staging experiences” for their patients, building colorful, fantasy-inspired atriums and play areas to create a fun and welcoming environment to distract from and offset the inpatient experience.
Modern service design offers a framework of methods for healthcare services, albeit one in which design is still seeking a perfect fit to practice. According to Birgit Mager, design professor and founder of the Service Design Network, service design thinking “addresses the functionality and form of services from the perspective of clients. It aims to ensure that service interfaces are useful, usable, and desirable from the client’s point of view, and effective, efficient, and distinctive from the supplier’s point of view.”8
Dubberly and Evenson saw services design evolving into complex experiences and systems, beyond client and user-centeredness.9 They propose designing for services by creating design languages for new service design. A design language provides a coordinating architecture for guiding the brand and process design and the ongoing evolution of a service project well beyond an immediate engagement. Design languages coordinate the provision of resources for co-creating value, the “staging of experiences,” whereby services actually touch the human experience of their interaction.10
Service design has developed well beyond the baseline of UX methods to multipoint service offerings and the creation of intangible value, such as positive emotional experience. Published service methodologies lead with a wide array of UX and adapted design methods. Yet little consensus is found across design disciplines with respect to service models in healthcare and, in particular, evaluation methods and standards of evidence. This matters because service design recommends specific methodologies for redesign of service processes but is primarily design-led, not research-led, and breaks from evidence-based tradition. The new modes of service design could be problematic in healthcare, or at best may focus on ineffectual changes and potentially slow the opportunity for healthcare service design.
For the past 40 or 50 years, service industries have traditionally relied on strong analytical methods, systems analysis, and operations research to make business-led design decisions for complex services. Yet healthcare is too complex to rely on just one field or methodology exclusively. No single school of design thinking is sufficiently comprehensive to be effective in all complex situations.
Service design aims to both enhance a consumer’s experience of the provider while also optimizing the design of service delivery and business transactions. But healthcare is neither transactional nor consumer-oriented, and the standard of evaluation (or care) is necessarily different than the standard for banking or travel planning. The rigorous research and evaluation of EBD might be considered the “standard of care” by which process changes are measured and claimed to be valid. UX and service design do not generally follow or publish scientific methodology in their delivery, as the risks for mistakes or system breakdown are not so hazardous in most domains.
Due to the high internal costs of clinical work, many of the technical efficiencies possible in clinical delivery have been identified, evaluated, and optimized. In clinical practice, the performance of a procedure is conducted thousands of times over, and technical inefficiencies have been driven out. This does not mean that the processes are perfected or even maximally effective, but more that the motivations for process change, being primarily regulatory or economic, have been satisfied or even optimized. Making further changes on behalf of patient experience is a new driver, and one with potential costs and risks. But these changes should not be merely branding or decorative in nature—positive health outcomes depend on deep knowledge of human physiology and behavior. Health services can link functions from the individual health seeker to the organizational level to radically improve service and the experience of care.
A Design Language for Care Service
A service is fulfilled when a change in condition is registered by the person receiving the output of an economic activity—a customer-supplier relationship. In designing for health, facilitating the effective change of a health condition is the primary goal. But no single design approach will serve and satisfy every service requirement. Not only are different methods necessary for the different types of healthcare modes and types of patients, but different philosophies, schools of methods, and consultation approaches are necessary for different service problems.
What is the target of service design? Is it the service clients expect? Is it a system platform for service delivery? The service systems view, according to IBM’s Jim Spohrer and service theorist Paul Maglio, defines service systems as “dynamic value co-creation configurations of resources (people, technology, organizations, and shared information).”11 These configurations create complex, nonlinear, socially organized processes. They are sociotechnical systems by another name. Service systems promote a strong focus on value co-creation, the proposition that value realized by the customer results from both the service offering and the customer’s interaction and use. The customer (the health seeker) is considered the source of value, and the interface with the service offer is where most of the designable value occurs. This service-oriented logic has the potential to change the institutional model as new healthcare organization forms are planned and, yes, designed.
A design language for sociotechnical services design might be evolved for healthcare. The drivers for a language (or just as well, a process model) are clear—creating better patient experiences for lifelong health value, enhancing clinical coordination at the appropriate scales of organization, reducing medical errors, and saving costs. A design language would enable us to form new service ecologies, integrating environments, processes, clinical functions, and HIT, and to integrate the capabilities in design to align with the life cycle of the health seeker.
Table 5.4 suggests a design language framework based on the Rheinfrank and Evenson concept. A specific set of design options and placements would be constructed for a given service. Here the basis of a service design model for co-producing health value is expressed in terms of the sociotechnical system elements necessary in a clinical application.
TABLE 5.4 A SOCIOTECHNICAL SERVICE DESIGN LANGUAGE
Service levels |
Design intent |
Service design elements |
Health seeker: Inpatient Outpatient Advocate |
Enable realization of health value proposition |
Public and media awareness, communications |
Patient–communications interface |
Enable awareness of health information |
Online content resources |
Patient–management interface |
Enable enduring care relationship with organization |
Direct correspondences |
Patient–clinical interface |
Direct care service relationship |
Health service experience |
Clinical care team: |
Develop strategic and procedural clinical abilities and resources for care service |
Socialization and team learning |
Clinical–management interface |
Enable design of resilient |
care services Care planning |
Clinical–information interface |
Enable effective clinical data, information, and knowledge management |
Access and usability |
Patient–life cycle interface |
Enable lifelong health habits and care activities |
Caring aftercare |
Patient–care circle interface |
Enable full life-cycle care after clinical services |
Educating patients |
Patient–payer interface |
Enable seamless billing and coverage |
Communication design |
The service design language represents an initial formulation of what Richard Buchanan called placements, positions where designed artifacts or intangible services are located in the flow of use. The designer is left to choose how to best create the placement: whether to make self-health booklets, a website, a personal relationship, or an e-mail campaign. For clinical procedures, the practicing physician would set the constraints, but a service design might identify related “touchpoints,” such as communications or room treatments, that facilitate a better experience.
Referring back to Figure II.1, we can map the design language elements as guides to placement along Elena’s patient journey. Her health seeking proceeds from being a family caregiver to having her first incident and her navigation of the health system for diagnosis and treatment. Her first touchpoints (primary care) are the examination and first orders at her doctor’s practice and her exchanges with friends about the hypothyroid medicine. As her awareness shifts to the need for self-care, her information seeking and communication paths become open to a wider range of information opportunities. Though conventional clinical processes would serve her well, the quality of care could be evaluated and enhanced along every dimension. This approach is defined by the Design 2.0 approach to service design—engaging clients and patients-as-users in rethinking care as a patient-centered service experience.
A Clinical Design 3.0 approach rethinks the patient experience as a continuity, integrated across organizations to facilitate full life-cycle care. Design 3.0 innovates by organizational transformation to plan changes in management, business models, and services to fulfill an envisioned value proposition. Whereas a single organization would improve care within its boundaries, an integrated practice can collaborate in a service system capable of integrating the primary, ambulatory, outpatient, and inpatient life cycle of Elena’s health-seeking journey.
DESIGN BEST PRACTICES
• Patient-centered design attempts to address all the touchpoints health seekers encounter, from medical care and medications to management and communications.
• The most complex design challenge is configuring end-to-end service centered around the health seeker. Today care is treated as a series of discrete events managed by different clinical offices. Advising, diagnostics, treatment, medication, and preventive care are not integrated.
• Clinical service redesign today is led by practices. Service design provides a framework for full participation across roles in the design of better processes and patient touchpoints.
• Become familiar with (and know how to select) multiple methods to ensure the best fit to a client problem.
Case Study: Patient-Centered Care Innovation
Much good work in healthcare service design is being done in European and Canadian jurisdictions. But we cannot easily translate service design solutions developed for a given national system. Ontario is starting to adapt the accountable care organization model from the United States for community care practices. But could the United States adapt Canadian clinical service design?
The Canadian system has some advantages from a service design perspective. A superior process can be taken from prototype to scale at the provincial level by evaluating its validity and efficacy in a service setting. This would be a challenge in the United States, where each “system” or major medical center manages its own processes and is not beholden to a larger system.
Public health becomes “more public” when a single funder can take regulatory responsibility for local or regional public health emergencies, vaccination or flu shot campaigns, and public messages to help inhibit the spread of infectious diseases or airborne pathogens.
Center for Innovation in Complex Care
Toronto’s Center for Innovation in Complex Care (CICC) is an institutional start-up, an innovation network formed among practitioners and researchers in Toronto’s University Hospital Network, Canada’s largest hospital center. The CICC operates as an open innovation group within the institutional structure, and organizes research projects with multifunction teams of physicians, nurses, pharmacists, industrial engineers, public health researchers, architects, residents, and designers. This diversity of knowledge and perspective gives the CICC an innovation advantage. Another significant factor in the CICC’s success is its direct, immediate access to the hospital’s internal medicine practice and patients. Barrier-free clinical access facilitates rapid testing of concepts and collection of data.
The CICC studies and enhances the entire process of complex care for patients with multiple disease conditions, which represents the largest burden on healthcare services. Physician and CICC medical director Dante Morra described its mission and approach to service innovation:
People see healthcare as one thing, and it’s not. There are three major streams of activity. The first one is the person going for an episodic treatment. For instance, they would need a hip replacement, and this can be done through one intense experience. This is like a manufacturing line, and it’s not complex. It’s one interaction, and if things go wrong there can be more interactions that follow. The second is the “well patient” in primary care. Sally is fine, but she is not feeling well, and she goes through the information and diagnosis phase. She goes back to her normal life.
The biggest mind-shift of healthcare happens when people start thinking beyond these two things. Most people have gone to their doctor with a flu, or they have had a major procedure done. When you look at the cost of healthcare, . . . if you look at the system, it’s all chronic disease. The chronic disease vortex is chewing up resources. The system is not designed for this.
And the real problem is not providing diabetic care to Sally. The provision of specific care is easy. The real problem is how to provide care to a patient who has diabetes, kidney disease, and heart failure. And who is alone. That is where the opportunity for design lies. This is the level at which CICC is looking to address problems.12
Using a bottom-up identification and innovation process, Morra and his staff work with clinicians, stakeholders, and patients to map out problems with current healthcare practices and develop and test solutions. The team’s direct access to the working clinical world allows for rapid observation, learning, and diffusion of knowledge.
The CICC created and follows an explicit, well-defined innovation strategy and a collaborative project management process. Handling more than a dozen clinical research and innovation projects at any given time, Morra and designer Leslie Beard coordinate weekly operational “rounds” to track and discuss the progress of projects. Just as in clinical education, the CICC staff refers to their weekly innovation project rounds as “bullet rounds,” similar to the quick review of patient cases residents take part in before visiting the patients in the circulating rounds. The CICC staff also hold regular invitational lectures for research findings as a type of “grand rounds,” the term for a prepared lecture based on the observations of a significant patient case in the clinic.
The innovation process draws from the everyday concerns raised by clinicians working in the University Hospital Network. As Morra explained,
We were formed to solve complicated problems. We started in the lean engineering methodology, value stream mapping with a heavy emphasis on process. But it stopped us solving the problems in this room. We may be able to solve the problem of how best to align the chairs in this room, but how do you align the chairs in the whole healthcare system? That’s where you need the design middle layer. 13
The Innovation Pyramid
The CICC relies on a well-defined innovation process to explicitly guide service innovations through a progression of stages so that efficiencies and economies of scale may be realized while accelerating learning and diffusion. Morra and Beard created the process with the CICC to provide a common language for practice innovation across projects, and Morra reinforces the progression “up” the scale for all projects. Morra often encourages research leads to consider how they might take a new process “to scale,” meaning the higher stages of diffusion:
- Understand the issue and create a project. Develop new understanding in order to disseminate new knowledge to improve processes with the goal of developing an intervention to change the existing system.
- Implement a pilot project. Implement on a small scale to gain an understanding of the barriers to moving forward, and to develop an initial structure for system enhancement.
- Evaluate the project. Determine the fit and feasibility of the process, and generate measures for full cycle review.
- Create a program. Develop a program that can be implemented or expanded by other teams to drive large-scale systems improvement.
- Commercialize. Disseminate the innovation into the marketplace and capture the value for society, the CICC, and/or the innovating team.
Even though the final phase is commercialization, the CICC is not structured to commercially develop innovations. Instead, the rationale of moving candidate projects from stage 1 to stage 5 is to diffuse innovations so they can have the maximum global system impact, a key mission of the CICC:
Having commercialization at the top is meant to represent saturation and breadth of influence that transforms the system. It’s not a higher order. The reason it’s at the top is that the opportunity for disruptive massive system impacts is in the marketplace. . . . The ability to truly transform a global system increases as you go up the pyramid. So if I am working with the Canadian government, I can create a program that can affect Ontario. It may not be able to be copied anywhere. But if I create a new gadget, that becomes BlackBerry RIM, that goes international. . . . it’s not more important, it’s just about the volume and amplification.14
Innovate Afib
AF is the most common cardiac arrhythmia, the incidence of which is growing as the population ages. This disease is a cause of significant mortality and comorbidity—that is, it co-occurs with other related disease conditions with age. As such, it is a significant problem for healthcare systems everywhere because of the burden on clinical care resources, especially when considering the “total system” costs of the disease beyond just AF care (estimated at between $20,000 and $40,000 per patient per year). According to the 2010 whitepaper by Morra and colleagues, AF accounts for 15% of all strokes, and patients are at a significantly increased risk of death due to stroke and heart failure.15
AF has a significant negative impact on a patient’s quality of life due to both its symptoms and the need for anticoagulation monitoring following diagnosis. AF frequently leads to palpitations, fatigue, heart failure, angina, and other conditions. The comorbidities of AF patients introduce complexity (interdependent relationships) into care decisions and disease management. Many patients suffer from diabetes, respiratory disease, and other chronic illnesses. They often see many specialists, take multiple medications, and interact with the healthcare sector at many points.
To better characterize and understand the nature of the challenges related to the disease, the CICC’s Innovate Afib project employed a multimethod analysis approach that included interviews with clinicians across the spectrum of care for AF patients, a systematic review of current literature regarding the cost of AF care, and validation of the system (and map) with key stakeholders.
Interviews were conducted with 60 thought leaders selected for their discipline and perspectives, including cardiology, pharmacy, internal medicine, primary care, AF clinic, systems, and nursing. These yielded some common themes and challenges with AF care in the current system:
• Fragmented care delivery
• Poor communication between providers
• Lack of follow-up with patients
• Nonstandardized care
• Confusing guidelines and lack of consensus on quality indictors; no clear entry point to the system
• Operational issues (wait times, new therapies)
• Lack of patient education
• Difficulties with patient self-management
• Challenges with patient adherence to therapies
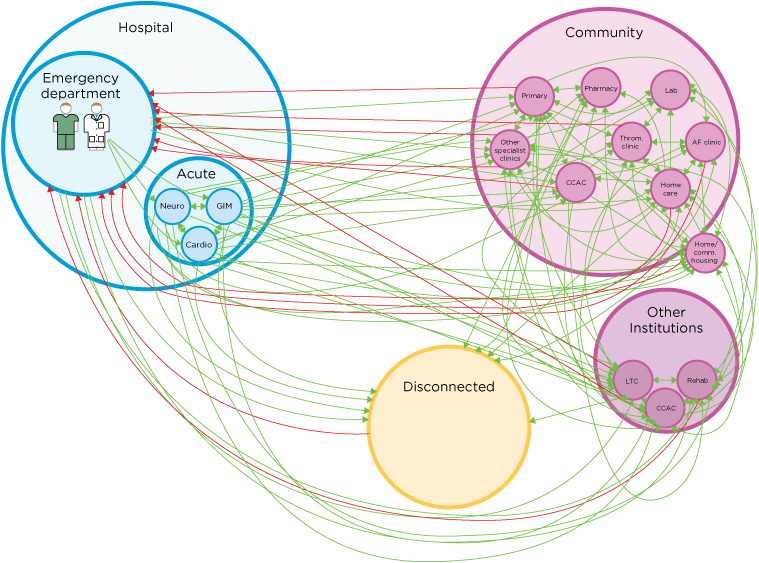
Associated with and resulting from these challenges, AF patients often experience a confusing care pathway, which may lead to (at best) basic symptom relief and prevention of further disease, or to deterioration (Figure 5.2). The way in which patients are managed in the existing system also results in increased utilization of resources, such as emergency room services, stroke rehabilitation services, and healthcare expenditures.
FIGURE 5.2
The existing network of disconnected atrial fibrillation (AF) services. AF patients flow chaotically among care providers. Disconnected patients are those who have been touched by the system but are now unaccounted for and may not be receiving proper care. This population is likely to end up in the emergency room. CCAC = Community Care Access Centres; GIM = general internal medicine; LTC = long-term care. (From Center for Innovation in Complex Care, Toronto)
An underlying assumption for the proposed new service process is the recognition that the healthcare system is in the midst of evolution—from delivery of episodic, fragmented care for individual conditions to multidisciplinary, team-based care of patients with multiple chronic medical conditions. As the general population ages, technologies change, and patients become more medically complex, taking a systems-based approach to managing this greater complexity will be the only way to provide comprehensive care that keeps people healthy and ensures that healthcare costs do not spiral out of control. Innovate Afib would reduce the system costs of the disease while simultaneously increasing the quality of care by reducing the complications of AF and improving efficiency and reducing redundancy.
Innovate Afib identified an “ideal care system” scenario (Figure 5.3) that would provide every AF patient with specialized anticoagulation management, around-the-clock patient access, follow-up within 1 week after any AF-related emergency room visit, access to specialist cardiologists when appropriate, and measured quality-of-care indicators. The diagram is read by observing the following six principles:
- The patient is at the center of the system, not the disease.
- Current referral patterns and existing infrastructures should be maintained and optimized.
- A value-based care model will reduce costs and improve care.
- Patient services should remain in their communities.
- Knowledge translation for physicians and patient self-management is provided.
- Communication is coordinated among all care providers.

FIGURE 5.3
Proposed integrated service network for atrial fibrillation (AF). CCAC = Community Care Access Centres (outer ring); CCC = Complex Continuing Care; CHC = Complex Health Centres; CSLS = customized supported local solutions; EI = existing infrastructure; GIM = general internal medicine; LTC = long-term care. Each of the bubbles can be customized per the CSLS model of local adaptation. (From Center for Innovation in Complex Care, Toronto)
At first glance, traditional designers and many readers may be unsure about where the possible design opportunities are found in this service scenario. Morra suggested that the best potential for high-impact innovations are in clinical and coordinated care processes: “Healthcare has been very innovative in creating new treatments, new drugs, new devices, new services . . . but not models and processes. What separates us from some of our colleagues is that they often try to create a product in one area. And if you want to create a product, you do not go into deep complexity. You carve out something small. But the problem is that products do not solve the true problems.”16
LESSONS LEARNED
• Innovators in a hospital ecosystem must formulate practices in language appropriate to the current stakeholders and keep the vocabulary limited to essential terms (e.g., the CICC presenting its projects in “rounds”).
• A well-defined innovation process helps clinical participants understand the common goals all share in the process.
• Service process design can advance the healthcare system toward its evolution from episodic, fragmented care for individual conditions to multidisciplinary, team-based care of patients with chronic conditions.
• Adapt a multimethod research approach, collecting traditional data (subjective report, measured observations) as evidence understood by sponsors. Clinical innovation benefits by publishing findings in medical journals, so a mix of EBD, design research, and clinical research methods can be used.
• Be prepared for clinical service design to take much longer than work in other domains. Agile processes are largely unknown in hospitals and are not recommended, as time to market is not a driver of innovation success. Effectiveness and risk/cost reduction are clinical goals, and quality and risk are compromised when optimizing for delivery time.
Methods: Design Research for Healthcare Services
Service design potentially represents a significant change and challenge to experience design and technology infrastructure design orientations. A comprehensive presentation of service-oriented design methods would fill another book.* Because the health sector is vast and by necessity conservative, a selection of methods for service innovation is meaningless without establishing a specific context. The integrated service design framework in Table 5.5 identifies the contexts in which the example methods stand.
TABLE 5.5 INTEGRATED SERVICE DESIGN FRAMEWORK
Design phases |
Methods |
Discovery/understanding |
Participatory workshops |
Human-centered research |
Ethnographic field research |
Service concept design |
Participatory workshops |
Process prototyping |
Bodystorming (simulating use cases) |
Service process integration |
Service blueprint |
Organizational readiness |
Service design plan |
Note: Methods are coded by color: innovation method; experience design research; social science research; systems method; service design method.
Although many methods referred to in this book are applicable to a service design context, the methods in this chapter are uniquely so.
Participatory Scenario Design
The participatory scenario design process elicits multiple perspectives and experiential knowledge from people with a deep understanding of the field. Facilitating scenario development as a workshop process helps participants form shared mental models of user behavior associated with the product/service design context. By formulating scenarios as a collaborative process, people get the chance to share their own stories, wisdom, experience, and details helpful to the group’s developing understanding. Such a shared understanding is more powerful than a set of storyboards developed in isolation by design researchers as a prepared deliverable. As a group’s understanding evolves and their stories become embedded in scenarios, the resulting story lines of shared knowledge become a basis for future design decisions, many of which will occur as business or product development decisions well in the future. Scenario design can be viewed as an investment in the long-term process.
Guiding scenario design requires setting the context for the activity, typically as part of a series of design workshop processes. A sequence of activities may be structured along the following lines:
- Review and discuss user and market research.
- Articulate themes and priorities from research to carry forward into design.
- Identify stakeholders and users from research and requirements.
- Engage the team in defining personas as a small-group exercise.
- Review personas and list relevant activities for each.
- Identify common activities across personas, and cluster personas into sets where it makes sense.
- Generate and sketch activity scenarios for high-priority persona activities.
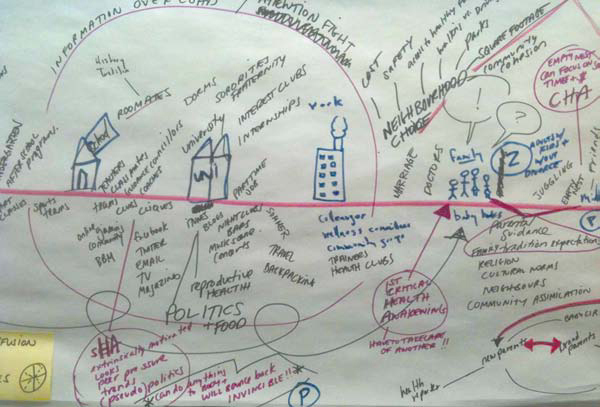
Scenario creation starts at step 7. Participants generally start either by posting anticipated actions and events on sticky notes to generate a series of touchpoints and potential encounters, or by creating a timeline for the period of engagement and associating events with time dependencies. Figure 5.4 illustrates the scenario construction of the former.
FIGURE 5.4
Creating a scenario of events and encounters for a health issue. (Sketch by George Shewchuk and Michi Komori)
Figure 5.5 illustrates the outcome of a timeline scenario. This shows the envisioned sequence of life events—from college to first job to middle age—to identify the points of intervention for health conversations. Although this is a much longer timeframe than a typical customer journey, the scenario process benefits from leaving the timeframe, experiences, and ideation open to the experience of participants.
Scenarios are generated for a set period (30 minutes is typical). A variation that is done within informed groups of varied roles or disciplines is to hold charettes of the first scenarios: A narrator stays with each team’s scenario while all others circulate around the room and walk through and critique each of the scenarios. New sticky notes (of another color) can be added to annotate the sketches with additional events, touchpoints, or suggestions. Following the development of rough sketch scenarios in the workshop setting, the narratives can be integrated into design artifacts and shared with management and the development team.
FIGURE 5.5
Timeline scenario for a health journey. (Timeline by Tai Huynh, Jen Recknagel, and Jayar Lafontaine)
Generative Bodystorming
Bodystorming is a well-known method for simulating and designing action sequences for services and interaction design. It allows the team and stakeholders to experience some of the functions and working relationships of proposals, either during their formation or after prototyping. It has been adopted and recommended in service design methods as a way to prototype the experience of interacting with an envisioned new service both physically and temporally. For healthcare services, which revolve around the physical performance of activities, bodystorming provides a way to run process simulations with real people for innovative concepts that might otherwise be prohibitive to prototype. Bodystorming identifies possibilities for innovation and tangible complications that would not be discovered in storyboards or computer simulations.
Because many services are largely intangible products that deliver values at points along the “service journey,” the typical prototyping approach is impoverished compared to interactive or industrial products. Very few services are fully tested as interactive prototypes with representative users, unless they are largely interactive services. Even then, consider a patient admissions process, for example. Although this is largely an online transaction for data entry, it also represents the patient’s first engagement with the healthcare center or system. The experience can be treated as businesslike and perfunctory, or as an opportunity to design a humane and orienting stage for a better experience. By default, if we let a critical process such as admissions follow the lead of an IT system, it promotes the worst aspects of the healthcare system in the patient’s first encounter, reminding the patient that care is a bureaucratic and expensive process.
Bodystorming can smooth out the rough edges of a designed service scenario. It simulates the touchpoints and interactions in actually performing the service, and animates scenarios so that teams can uncover potential problems and reveal hidden assumptions embedded in the prototype. At least four bodystorming techniques have been documented for different purposes and different stages of a design engagement:
• Designing in situ. This is bodystorming with the development team working in the space or place in which the product being designed will ultimately be used. Although this could be a valuable experience for designers, it would be difficult to carry out in a working care setting.
• Service simulation. This is bodystorming as “strong prototyping” to represent the environment and local situations in which the product or service will be used. For example, a team has been hired to build a new handheld device for use on submarines, so they construct and model the hallways, spaces, and structures (out of cardboard perhaps) to simulate a submarine environment. It may not have all the properties of the actual field setting, but might appropriate the most salient objects. The team can change variables, such as lighting, or test how easy it is to walk through doorways and passageways of different sizes while trying to use the handheld.
• Use case theater. This classic bodystorming technique prototypes the space and place of service by using living personas, actors, and props.17 In a wait time reduction scenario, a team might test their scenarios for improvement by simulating and timing the interactions of queues, entry and exit conditions, clinical procedure variances, and information collection. The design team would define service scenario scripts, rehearse the scripts so that performances were evenly conducted, and measure the time needed to service the queues under different test conditions. This technique is used more in an evaluative context, and is conducted in later stages of design.
• Embodied storming. This technique differs from the others in that the goal is to create embodied perceptions of use and interaction for a future service.18 This approach is a pre-ideation technique, in which perceptions based on gut feeling precede the pursuit of perfect concepts. The design team improvises and learns from the observations of their experience in trying out the situation being designed for.
These techniques are not mutually exclusive, although they are almost never used together on a design project because they are useful at different times in the design process.
Embodied storming goes beyond just the creation of a “simulation” and allows the real-time generation of new scenarios that would not otherwise be considered. The technique is staged as a generative tool for creating insights that precede ideation and concept design. Early bodystorming also helps a team discover flaws and assumptions before brainstorming and concept development.
Embodied bodystorming requires people to act as physical actors in a situation, and not as conceptual designers distanced from things. Stakeholders and designers work in artificial situations when developing design concepts, becoming blind to perception (i.e., personal experience of an event) and instead focusing on the facts of representation (i.e., after the event). Bodystorming enables rapid communication between people, and the generation of unjudged, uncompromised proposals and scenarios. The performative mode tends to create sequences, themes, and conceptual continuity. They are like scenes composed by a “design troupe” rather than discrete ideas attributed to individuals. Ideas can be elicited from the scenario, but extracting them in isolation tends to disrupt the continuity of the scenario.
Generative bodystorming helps to create stories or themes from the service experience, based on the things and situations being perceived and observed. It enables translation of tacit knowing into rapid communication and generation of ideas contributing to the service scenario. By collaborating in tight generate/do/learn cycles, participants engage one another in simulating experiences and processes that are designed through joint acting and improvisation.
The distinctions between use case bodystorming and embodied storming listed in Table 5.6 show the value of this technique in service design.
Interaction design relies on personas as a way to represent users as the subjects for product design. Yet service scenarios represent dynamic coordinated activities, sometimes across a wide range of persona types. For example, a patient may only participate in the touchpoint of a tangible interaction with a service’s delivery, such as a prescription being filled. Behind the scenes, the service involves multiple backstage actions with tangible items and intangible functions the patient never sees, such as physicians’ orders, professional communications, computer entries, and movement of supplies and medications. These activities are not represented by persona types, and their service moments are not personalized—they are necessary interactions in a service workflow.
TABLE 5.6 USE CASE AND GENERATIVE BODYSTORMING
Use case bodystorming |
Embodied storming |
User-needs centered |
Rapid communication and generation of ideas around an envisioned scenario |
Product-design driven |
Developing people and cultures through shared understanding |
Creative problem solving/design thinking on site to enhance understanding of the problem domain |
Rapid communication and generation of ideas around what the problem domain should be |
Focus on physical problems |
Problems are not always technological; sometimes they are sociopolitical or socioeconomic |
Reenacting people’s everyday performances and living with data in embodied ways by performance |
Envisioning how people would respond to future scenarios that are presented without extra data |
Quality of design ideas is heavily dependent on the quality of documents |
Quality of the exercise is dependent on the quality of interactions and breakdown of cognitive and emotional barriers |
Participants are researchers and industry representatives |
Participants may not know anything about the subject area |
Success is measured by the uptake of ideas by industry representatives |
Success is measured by participants’ willingness to explore together and build shared meaning around issues |
Empathy toward users |
Shared experiences and collective memory |
Role-playing and following a script |
Free flowing, not directed (aside from presented scenario) |
Forced innovation of solutions |
Exploratory but not solution driven |
Personas can be a helpful tool for understanding the varying needs of different user archetypes, but they can be a crutch in service design situations.19 Services must be designed and specified to enable an unforeseeable range of individuals to interact readily, easily, and fairly with a given service system. Focusing on personas too closely skews the consideration of need states—conditions of a situation that require satisfaction or reveal a breakdown. Although scenarios portray the interaction, information flows, and touch-points of service, they do little to demonstrate the human responses to a service system design. The emotional and behavioral responses to a time-pressured, human-system need state can be played out as theater, with the impact of immediate and shared insights into the situation.
Generative bodystorming focuses on need states and can be applied as a design research method to help identify gaps and opportunities. A typical scenario finds design teams sitting around the table and talking about users as if they were segments “out there” waiting for us to discover their so-called needs. We classify customers by demographics such as age or gender, psychographics such as lifestyle, and behaviors such as purchasing patterns that we believe to be real enough to measure. If well funded, we go “out there” to conduct research on these different segments. Instead, or in addition, the projective role-playing of embodied storming forces a team to attend to perceivable need states.
A single product or chain of service events might generate multiple need states. Because a product cannot serve all needs, we use embodied storming to focus on the needs that matter. If performed with a reasonably informed troupe, embodied storming will demonstrate the satisfaction of the conditions of these need states. An effective bodystorm is one that captures the need state, highlights the breakdowns, and shows how the change in process (the designed aspect) satisfies the problems as perceived. A good bodystorm has an immediacy and intimacy that engages clients and participants at a direct level of experience with respect to the real-world situation for which the team is designing.
We need to focus more on the different usage occasions with the product and service, and the needs that define them. This is exactly what bodystorming does. It goes even further because it allows us, both as designers and business owners, to see and understand what is and what is not working so that we can interpret design opportunities.
Guidelines for Generative Bodystorming
Guidelines for embodied storming are not rules because the technique is still exploratory and remains in continual practice.
- Expect to spend 2 to 4 hours planning and designing the bodystorming scenarios, materials, instructions, and logistics. A series of bodystorms to evaluate different proposals requires more planning.
- Assign five to eight participants per troupe. Larger groups can be split into two or more troupes that bodystorm the same scenario.
- Every player must have a role; there are no background players.
- Identify and create props for use in the scenarios. Props can have feelings and thoughts, and are interactive agents in the process.
- Create large cards that identify the roles.
- Create thought-bubble cards to show what a participant is thinking versus saying or doing.
- Have a narrator or color commentator who explains things to observers. The narrator can stop the action, rewind, or fast-forward.
- Approach the presentation of scenarios with the spirit of improv acting: “Yes, and . . .” rather than “No, but . . .”
- Perform at least two skits, showing a before and after service scenario.
TIPS ON TECHNIQUES
• In the right context, any user-centered design method can be applied in healthcare service design. Sequence a series of research methods so they contribute significantly to each design decision.
• Participatory methods such as dialogic design and bodystorming are especially useful in co-creating and proposing new service interventions. Methods that result in consensus diagrams, such as challenge maps, enable collective understanding and enable managers to articulate clear proposals.
• Design research methods can blur the boundaries and nudge practitioners into making proposals for which their experience is inapplicable. Service designers without clinical experience should avoid advising on clinical content. Methodologies such as dialogic design and Simplexity make a clear separation between process facilitation and practitioner content.
• Generative techniques such as embodied storming provide an alternative to prototyping services. Because so many variations of possible activity are possible in a service available to all types of health seekers or professionals, the embodied methods allow designers to understand the complexities of an intangible service from a physical and temporal perspective.