Chapter 4
Application of Epidemiological Concepts to Health Care Delivery
Learning Objectives
- Comprehend the major uses of epidemiology in the restructuring of the health care delivery system
- Become aware of the value of epidemiology as an adjunct to making medical decisions
- Understand the value of information management in the improvement of health outcomes
- Recognize the use of epidemiology in determining best practices in health care delivery
Epidemiology has been part of both medicine and public health since the first recorded outbreak of disease. Epidemiologists examine the health of the population, not the health of the individual—a practice often referred to as population-based medicine. Epidemiology has served public health departments well over the years by helping solve many of the mysteries surrounding the causation of morbidity and mortality associated with communicable and noncommunicable diseases. The principles of epidemiology are now being applied more widely for use in medical decision making, and should be particularly helpful as we reorganize the health care system. A very important piece of the new world of public health is going to be the expanded use of epidemiological tools to investigate the problems inherent in combating complicated chronic diseases and implementing evidence-based prevention programs.
Hippocrates, who lived between 460 and 377 bce, probably made the first use of epidemiology when he recorded outbreaks of such communicable diseases as plague, cholera, and dysentery. As the science and art of epidemiology grew in stature and understanding, its many possibilities in the scientific field also expanded. In recent years those working in health care management positions have used epidemiology to solve many managerial and marketing problems. Its important place in medical decision making is evident in that it has become a vital component of the graduate curriculum in health care administration programs around the world.
Epidemiology is a sound method of data gathering and investigation that employs statistical techniques to evaluate hypotheses concerning the causation of any given disease or health problem (Merrill and Timmreck, 2006). Investigators, or medical researchers, frequently use the epidemiology of chronic diseases, injuries, environmental and occupational exposures, and personal behaviors. There is no reason why the science of epidemiology cannot be expanded for use in offering solutions to many of the major problems found in our current health care system. Merrill and Timmreck (2006) further define epidemiology as the study of the determinants, distribution, and frequency of disease.
Like a detective methodically solving a crime, the epidemiologist attempts to understand a disease by determining the various causative factors. Detectives work with motives, circumstances, and profiling of the victim and the criminal; epidemiologists analyze the disease, injury, or other health problem, and profile the victims and circumstances—the environments, habits, and motivations for healthy or unhealthy lifestyles. Epidemiologists evaluate ill and well individuals in an attempt to find the reasons some people become ill and others do not. They usually begin this type of investigation by gathering data from ill and well individuals through surveys. They then attempt to uncover the determinants of the disease, and document locations and numbers of old and new cases. The data investigators gather from potentially exposed sick and well individuals allows them to develop a rough hypothesis to explain the causes of the problem.
The epidemiologist now begins building a case definition, which includes standardized criteria for determining whether a person has a disease or other health-related condition (Turnock, 2007). This case definition also incorporates clinical and personal qualities of the health event under investigation, eventually becoming the problem statement applied to that health event. Health care managers can also use this tool when gathering other types of health data that will help improve our health care system.
An epidemiological study can also be the starting point for a plan to control and prevent occupational injuries and disease. The first thing epidemiologists would need would be a well-defined case definition for each of the possible health hazards found in the various businesses throughout the United States. This would allow them to label health events according to location, time, and person, lending a degree of standardization to the process of investigation.
A good understanding of the principles of epidemiology can be beneficial to managers in all facets of health care management. It is really a science of decision making that is very useful for anyone faced with clinical or managerial responsibilities in health care.
The field of descriptive epidemiology involves the characterization of events such that investigators can explore common traits exhibited by those who are ill. By describing health problems according to time, place, and person, the epidemiologist is better able to communicate those problems in terms that can be understood by all (Merrill and Timmreck, 2006). Therefore, descriptive epidemiology allows public health departments to determine who is at risk of developing a particular health issue, enabling agencies to evaluate the proposed method of preventing that adverse health outcome. It is the most basic form of epidemiology, but it has great value when beginning to investigate a health event. The individual using descriptive epidemiology simply describes what happened in a way that makes sense of the available data, helping to offer a possible explanation of phenomena. This form of epidemiology is useful for evaluating any problem, not just an outbreak of disease.
Exhibit 4.1 is a list of diseases whose appearance must be reported to the Pennsylvania Department of Health. According to state law, medical facilities and physicians who examine and treat patients have to report these diseases whenever they encounter them. Efforts by this and other public health departments to deal with communicable diseases have as their goal the treatment of infected individuals and the discovery of new cases of disease in order to reduce the incidence of disease and protect communities from an epidemic. Through thorough investigation, epidemiologists and public health professionals are able to trace the step-by-step process of a disease's development.
Exhibit 4.1: List of Reportable Diseases
1. AIDS (Acquired Immune Deficiency Syndrome) $
2. Amebiasis
3. Animal bite #
4. Anthrax #
5. An unusual cluster of isolates
6. Arboviruses (includes Colorado tick fever, Crimean-Congo hemorrhagic fever, dengue, Eastern equine encephalitis, St. Louis encephalitis, West Nile virus infection, Yellow fever, et al.) #
7. Botulism (All forms) #
8. Brucellosis
9. Campylobacteriosis
10. Cancer ˆ
11. CD4 T-lymphocyte test result with a count <200 cells/microliter, or a CD4 T-lymphocyte % of <14% of total lymphocytes $
12. Chancroid
13. Chickenpox (Varicella) (Effective 1/26/05)
14. Chlamydia trachomatis infections
15. Cholera #
16. Congenital adrenal hyperplasia (CAH) (<5y/old)
17. Creutzfeldt-Jakob Disease
18. Cryptosporidiosis
19. Diphtheria #
20. Encephalitis (all types)
21. Enterohemorrhagic E. coli # *
22. Food poisoning outbreak #
23. Giardiasis
24. Gonococcal infections
25. Granuloma inguinale
26. Guillain-Barre syndrome
27. Haemophilus influenzae invasive disease # *
28. Hantavirus pulmonary syndrome #
29. Hemorrhagic fever #
30. Hepatitis, viral, acute and chronic cases
31. Histoplasmosis
32. HIV $
33. Influenza (laboratory-confirmed only)
34. Lead poisoning #
35. Legionellosis #
36. Leprosy (Hansen's Disease)
37. Leptospirosis
38. Listeriosis
39. Lyme disease
40. Lymphogranuloma venereum
41. Malaria
42. Maple syrup urine disease (MSUD) (<5y/old)
43. Measles (Rubeola) #
44. Meningitis (all types—not limited to invasive Haemophilus influenzae or Neisseria meningitidis)
45. Meningococcal invasive disease # *
46. Mumps
47. Perinatal exposure of a newborn to HIV
48. Pertussis (whooping cough)
49. Phenylketonuria (PKU) (<5y/old)
50. Plague #
51. Poliomyelitis #
52. Primary congenital hypothyroidism (<5y/old)
53. Psittacosis (ornithosis)
54. Rabies #
55. Respiratory syncytial virus
56. Rickettsial diseases/infections (includes Rocky Mountain Spotted Fever, Q fever, rickettsialpox, typhus, Ehrlichiosis)
57. Rubella (German measles) and congenital rubella syndrome
58. Salmonellosis *
59. Severe Acute Respiratory Syndrome (SARS) #
60. Shigellosis *
61. Sickle cell hemoglobinopathies (<5y/old)
62. Smallpox #
63. Staphylococcal aureus, Vancomycin Resistant (VRSA) or Intermediate (VISA) invasive disease
64. Streptococcal invasive disease (Group A)
65. Streptococcus pneumoniae, drug resistant invasive disease
66. Syphilis (all stages)
67. Tetanus
68. Toxic shock syndrome
69. Toxoplasmosis
70. Trichinosis
71. Tuberculosis, suspected or confirmed active disease (all sites) including the results of drug susceptibility testing
72. Tularemia
73. Typhoid fever #
For health care practitioners and health care facilities, all diseases are reportable within 5 workdays, unless otherwise noted.
# Health care practitioners and health care facilities must report within 24 hours.
For clinical laboratories, all diseases are reportable by next workday, unless otherwise noted.
$ Clinical laboratories must report within 5 days of obtaining the test result.
* In addition to reporting, clinical laboratories must also submit isolates to the state laboratory within 5 workdays of isolation.
ˆ Hospitals, clinical laboratories, and health care facilities must report within 180 days.
Source: Pennsylvania Department of Health. (PA Code, Title 28, Chapter 27 | Updates 1 & 2 requiring electronic reporting.)
The epidemiologist operates using a concept called the chain of infection to explain how disease is transmitted from an infected individual to someone who is not infected. It is a time-tested method used to solve medical problems with no known cause. Figure 4.1 shows the chain of infection for disease. A disease usually follows a step-by-step process, from infection to the manifestation of the signs and symptoms that become present with communicable and most chronic diseases. Documenting this process helps public health departments better understand how a disease develops and spreads from person to person.
The investigation of a disease also enhances our understanding of its major components, better known as the triad of disease: agent, host, and environment (see Figure 4.2). It is the intersection of these three factors that usually leads to the occurrence of disease. The agent is the cause of the disease, the host is where the agent lives, and the environment surrounds the host.
The starting point in the investigation of any problem is an observational study (Webb, Bain, and Pirozzo, 2005). In this type of study the investigator does not intervene in the problem being explored, but merely observes and records what is happening. Such observational studies can further be classified as either descriptive or analytical. Those using descriptive epidemiology are looking for common patterns of disease or other health problems.
One of the most famous uses of descriptive epidemiology occurred in 1854 during a London cholera epidemic. John Snow, a physician, used epidemiological techniques to observe the spread of cholera through the water supply coming from a water pump located on Broad Street. Prompted by knowledge acquired during his prior years of observing and describing the transmission of cholera through contaminated water, Snow surveyed households of cholera victims and traced their water supply to one of the town's three wells. Once the suspect well was closed at his urging, the illness in the town ended. This is one of many instances of the successful use of epidemiology to suppress an outbreak of a communicable disease.
Once descriptive epidemiology is completed there are several types of studies that can help prove causation in epidemiological investigations, many of which are conducted in order to follow up on associations that are suspected during the practice of descriptive epidemiology. Merrill and Timmreck (2006) maintain that randomized controlled trials are the most scientifically rigorous. These are experimental studies and usually fall at the end of a sequence of less-demanding and less-costly studies, which have already helped investigators develop a hypothesis about causation that will usually require more work to prove. These studies are very complex and expensive in their development, implementation, and evaluation. Therefore, descriptive epidemiology is usually the best starting point for investigating any health problem.
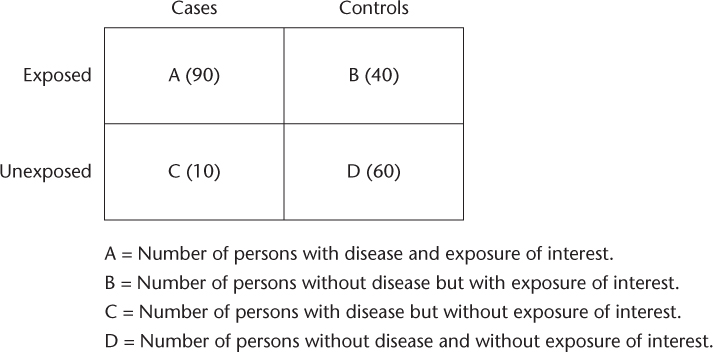
A case control study involves looking at retrospective data on both cases and controls in an attempt to determine the cause of the event under observation. According to Christoffel and Gallagher (2006), the case control study allows investigators to perform an odds ratio—a representation of the odds in favor of individuals' incurring a disease or injury when an associated factor is present.
An outbreak of a communicable disease has always been a serious concern for communities in this country. A communicable disease, also called a contagious or infectious disease, is capable of being transmitted rapidly from one person to another as well as from contaminated foods or water. Communicable diseases have been around since the beginning of time, and although their incidence has declined, they still are capable of causing panic in communities, schools, or workplaces.
Using descriptive epidemiology is a very rapid way to determine the criteria for cases and then select experimental controls from the pool of individuals who remained well after exposure, and discover the cause responsible for the outbreak of illness. Once the cause of the health problem is determined using epidemiological principles, control measures can be implemented to stop the problem. For example, frightening outbreaks of typhoid fever, cholera, and influenza have become more infrequent thanks to clean water, better personal hygiene, and the united efforts of environmental and public health specialists dedicated to controlling these past killers.
The success in controlling most communicable disease outbreaks has resulted in a relaxed attitude concerning the possibility that these diseases could ever return. One the one hand, we must remember that although most of these pathogens are under control, they have not been destroyed. In fact, only one communicable disease, smallpox, has actually been eliminated, despite the best efforts of public health professionals. On the other hand, descriptive epidemiology allows us to better evaluate any problem—new or old—and look for clues as to why the problem exists and what its solution might be.
Epidemiology of Communicable Diseases
As we have already noted, the epidemiology of communicable diseases has been studied since ancient times. Hippocrates, in an essay titled “On Airs, Waters and Places,” actually suggested that environmental and host factors were at the root of many diseases. Scientists have always been interested in how disease agents are spread from one person to another. McKenzie, Pinger, and Kotecki (2005) define communicable diseases as those caused by biological agents and spread to others, usually in a short period of time.
It bears mention that a number of diseases that are spread from person to person can also be classified as chronic diseases if they remain for a long period of time, as does tuberculosis. They can be acquired from another person, but can last for a long period of time. The best examples of such chronic and communicable diseases are acquired immune deficiency syndrome (AIDS) and tuberculosis (TB). AIDS is caused by the human immunodeficiency virus (HIV), which is spread from person to person by certain high-risk behaviors. It is considered a chronic disease, because once infected there is no cure, and the infected person will probably live for many years with the disease before he or she dies. Similarly, TB is caused by a bacterium that is spread from person to person; it becomes a chronic disease as time passes, and remains with the infected for an extended period.
The acute diseases that are easily transmitted from one person to another represent a serious threat to individuals in the workplace. The threat may include the dangers of illness and perhaps death, not only for the worker but also for family members, should that worker bring the disease home. The threat also manifests itself in a fear of the unknown, because communicable disease occurrence is a very rare happening, and nonmedical people often do not know the full extent of what exposure to a communicable disease means.
An agent is the catalyst that must be present for a disease to occur. If the agent can be eliminated, the disease usually caused by the agent will not appear. For example, poultry products quite often are contaminated by salmonella, a bacterium. If the contaminated poultry is cooked at the right temperature for the appropriate amount of time, then the agent is destroyed and no one consuming the product will also consume salmonella. This agent must be present for a disease to appear. Many such agents are well-known and occur on a frequent basis among individuals. Most people have heard of bacteria, viruses, and even protozoan parasites. Unfortunately, most people are unaware that these agents can be deadly, and also that they can be spread to others very easily under the right circumstances.
Public health departments are responsible for controlling outbreaks of disease caused by these agents. In fact, communicable disease control programs have always been a mandated public health function in all health departments throughout the country. The word control has been used in association with these agents because they have never been eliminated. They may be transmitted in different ways, their incidence may remain low, but they are always present and capable of causing large outbreaks of illness that can terrorize a community.
Communicable diseases are spread in a very specific way that epidemiologists and other medical personnel have studied for hundreds of years (McKenzie, Pinger, and Kotecki, 2005). Research into the chain of infection for various illnesses has been useful in developing an information base concerning the majority of infectious diseases that occur frequently throughout the world. Public health epidemiologists who investigate outbreaks of infectious diseases complete reports of their investigations and share them with other health agencies and the medical community. The Morbidity and Mortality Weekly Report (MMWR) offers up-to-date information on outbreaks of communicable diseases in reports written by disease investigators, helping medical personnel and public health professionals better understand how infectious diseases are spread from one person to another.
If any piece of the chain of infection is broken, the disease in question is stopped from spreading to a new host. This has been the case with vaccine-preventable diseases. If an individual is properly immunized and then exposed to the disease, there is no infection because the exposed individual is no longer susceptible to that particular disease.
The mode of transmission is the way an infectious agent travels from an infected person to a new person who is currently not ill. The route of transmission can be either direct or indirect. Direct transmission involves immediate transmission of an infectious agent to a new host, whereas indirect transmission may involve the air, a vehicle, or a vector (McKenzie, Pinger, and Kotecki, 2005). Indirect transmission usually involves an inanimate object, or fomite, is not immediate, and causes a panic situation among individuals who believe they may have been exposed.
Epidemiology of Emerging Infections
The resistance of some pathogens to antibiotics and the importation of diseases into this country from around the world have produced new and emerging communicable disease threats. Satcher (2006) argues that infectious diseases maintain a large reservoir of agents that are always available to create epidemics under the right conditions. Recent large outbreaks of infectious diseases like tuberculosis in this country underscore how easy it is to have an epidemic if public health professionals do not remain vigilant about the threat of disease. As discussed in the previous section, many infectious diseases, although they are currently under control, remain capable of reemerging as major health threats to the United States and the world.
One example illustrating the serious nature of these infectious diseases occurred in Milwaukee, Wisconsin, in 1993. Contamination of the water supply in this city resulted in an outbreak of cryptosporidiosis that affected an estimated four hundred thousand people, resulting in over four thousand requiring hospitalization. On a broader scale, TB reemerged in the United States in the 1980s as a formidable disease threat, especially in cases of drug-resistant strains. E. coli has also become a major threat to the public in recent years. Finally, pneumonia and influenza cause tremendous morbidity and mortality every year, and mutations of the influenza virus—like avian flu and swine flu (H1N1)—pose the threat of worldwide pandemics of disease capable of reaching this country and killing thousands.
The epidemiological approach has over time been employed to investigate chronic diseases that are noncommunicable; have long incubation periods; and have no cure once developed, usually resulting in serious and costly complications. Many of the chronic diseases are the result of practicing poor health behaviors like using tobacco, maintaining a sedentary lifestyle, and having a poor diet. The major reason for our escalating costs in health care in this country involves an epidemic of chronic diseases that require prevention, not a cure.
Moving beyond descriptive epidemiology, investigators use the techniques of analytical epidemiology in an attempt to prove the cause of a given health event (Webb, Bain, and Pirozzo, 2005). Proving causation is the major objective of analytical epidemiological studies. Rothman and Greenland (2005) argue that the ability to make causal inferences is self-taught, and that we learn about causation at a very early age through our own life experiences. For example, when we are young we learn that certain behaviors are praised whereas others are not. These authors then define the differences between sufficient and component causes of an occurrence. A cause, in general, is a condition that was necessary for a certain outcome, in this case a health problem. A sufficient cause is an event that by itself can cause an outcome. A component cause is one of several events that must occur in some order to lead to an outcome. The strength of the causal relationship, if high, usually offers an incentive for more researchers to study the cause or causes. The result repeated through several well-run studies offers stronger support to their final determination of the root of the health problem.
Analytical epidemiology involves using data to test hypotheses (Merrill and Timmreck, 2006). Analytical epidemiologists, for example, make comparisons between those with a disease or condition and those without the disease or condition, who had previously been identified through the use of descriptive epidemiology, quantifying associations of variables being observed and determining the cause or causes of the given problem. An analytical epidemiologist uses a comparison group to test the strength of the association between exposure and a disease variable.
Figure 4.3 shows an example of a matrix that displays study outcomes and is very useful in analytical epidemiological studies. (This matrix compares using tobacco and not using tobacco.) This table incorporates cases and controls who were either exposed or not exposed to the variable under study. A very good example of the use of analytical epidemiology is seen in a study conducted by Doll and Hill (1950) that implicated the use of tobacco in the development of a rare form of cancer at that time, lung cancer. This landmark study paved the way for additional chronic disease studies that linked secondhand smoke to the same deadly form of cancer. Tobacco became identified as the leading cause of death for 430,000 Americans every year (Centers for Disease Control and Prevention [CDC], 2008d). Secondhand smoke was also found to be a cause of over 80,000 additional deaths from lung cancer. This association has been very visible for a number of years, and epidemiologists have described it thoroughly in the medical literature. The maturing principles of epidemiology can now be applied in the investigation of other chronic diseases in this country, with the goal of preventing of these chronic diseases and their complications.
Figure 4.3 Sample Matrix Displaying Study Outcomes
Source: U.S. Department of Health and Human Services, CDC (2010).
After Doll and Hill's study (1950), it seemed like a natural follow-up to start using epidemiology to evaluate high-risk health behaviors as potential causes of other chronic diseases. The Framingham Heart Study, beginning in 1948 in the town of Framingham, Massachusetts, did just that. This cohort study involved 5,209 men and women between the ages of thirty and sixty-two who were initially free of coronary heart disease (CHD). The study followed residents of this town for over fifty years in order to discover how people develop heart disease.
Turnock (2007) refers to the twenty-eight thousand residents of Framingham who volunteered for this first longitudinal study of heart disease as having given a gift to this country. This study evaluated the effects of blood pressure, blood triglyceride and cholesterol levels, age, gender, and psychosocial issues on the development of CHD. The Framingham study was instrumental in helping to define the term risk factor as it relates to heart health.
This study revealed that by changing a few health behaviors—for example, by quitting smoking, maintaining a better diet, losing weight, and being physically active—one can reduce the chance of developing heart disease. The success of this study signaled that epidemiology was moving rapidly into the important and complex area of chronic disease causation. Epidemiology was now ready to deal with diseases with very long incubation periods and no visible starting point. As a consequence, the epidemiology of chronic diseases was now becoming a crucial part of public health departments in the United States.
One of the most feared words in the epidemiologist's dictionary is epidemic. This much-abused term simply indicates more cases of a certain disease than one would normally expect. The word epidemic can be used in the context of communicable and chronic diseases, injuries, and environmental and occupational health problems. Rowitz (2006) classifies an epidemic according to “the level of contagiousness, small facts or events that have large and long-lasting consequences, and how to prevent additional cases which can occur suddenly or at a dramatic moment.” Examples of epidemics are all around us on a daily basis. The city of New York is suffering from an epidemic of diabetes, the nation has prepared for an H1N1 pandemic, women are experiencing an epidemic of heart disease, and some occupations are undergoing an epidemic of homicides. All four of these epidemics can be prevented with the help of public health expertise.
The epidemiologist has many tools that are helpful in determining the cause of an outbreak of disease. One of the most important tools an epidemiologist uses in an investigation is a rate. In fact, it is noted by those in public health that what separates epidemiologists from other scientists is their comparison of rates in order to develop and test a hypothesis. A rate is a measure of some event, condition, disease, injury, or illness in relation to a unit of population during some specific time period.
It makes it much easier to compare health events if the population exposed and infected is taken into consideration. The rate of illness, disease, or injury is easier to comprehend if evaluated in terms of some type of morbidity rate. A morbidity rate is the rate of a given illness in a certain location during a certain period of time. A comparison of the causes of death makes more sense if the health event is evaluated in terms of mortality rate. Many of these rates are used when describing health events in the workplace.
Epidemiologists use many other rates in making comparisons within communities. The incidence rate, for example, is useful in a short-term evaluation of a developing epidemic of some type of illness. This rate is a calculation of the number of new cases of some illness over a short period of time. Further, the prevalence rate is a measurement of disease over a longer period of time, such as a year. The rates most important to an epidemiologist when investigating a disease or other illness are the incidence rate, prevalence rate, and attack rate.
Epidemiology and the Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention (CDC), headquartered in Atlanta, Georgia, employs over eight thousand health professionals, who are involved in health surveillance designed to monitor and prevent disease. The CDC is also responsible for the preparation and distribution of health statistics for the nation. This federal agency develops sophisticated epidemiology systems and provides training and certification programs for those employed as epidemiologists in the United States and several other countries throughout the world.
The founder of the use of epidemiology at the CDC was Alexander Langmuir in 1949. He was the main epidemiologist for the CDC for over twenty years, and helped to develop the Morbidity and Mortality Weekly Report (MMWR), which is responsible for reporting regularly on disease prevalence and current outbreaks (CDC, 2009b). This agency was a descendant of the wartime agency Malaria Control in War Areas, and its original focus was on the effort to fight malaria by killing mosquitoes. The initial budget was under $10 million, but over the next fifty-plus years the CDC developed into the nation's premier health promotion, prevention, and preparedness agency and a global leader in public health. It is the world leader in health data management and expertise in epidemiology.
Data management is the collection and analysis of information and the sharing of data with multiple audiences. Aschengrau and Seage (2003) point out that a great deal of information is available concerning diseases, injuries, disabilities, and mortality, much of which it is the responsibility of public health departments to manage and disseminate in order to the improve the health of various populations—such as those of cities, counties, and states—rather than individual patients. According to Webb et al. (2005), a very large part of public health practice is acquiring and disseminating information about a community in order to better understand the overall health of the group being studied or evaluated. Many of the health data are gathered and analyzed using the principles of epidemiology. Such data management has always been a required function of public health departments at the federal, state, and local levels.
Morbidity represents the incidence or prevalence of disease in a given population during a specified period of time. As discussed earlier in the context of rates, the incidence of disease is the number of new reports of disease, whereas prevalence usually refers to the number of reports of disease over a longer period of time. These data are available from physicians and laboratories, and federal and state law supports the right and obligation of public health departments to receive reports of certain diseases when they occur. Local or state public health departments then report these diseases to the CDC. The sheer volume of these data is enormous, but the information needs to be gathered and analyzed in a systematic way. These morbidity data were made reportable in 1878 when the U.S. Marine Hospital Service was ordered to collect reports on certain diseases that could easily be spread from person to person.
The term mortality refers to the deaths that occur during a given period of time. A pioneer in the gathering and reporting of mortality data was the seventeenth-century English epidemiologist John Graunt. He published the Bills of Mortality in 1662, which was a weekly count of deaths in London. The reporting of these data allowed him to categorize deaths according to their cause.
Public health data can be invaluable in completing a community health assessment, which usually includes the health data for a given population (Novick, Morrow, and Mays, 2008). The CDC is a major source of all types of data, many of which can help in the evaluation of preventive measures. These include health outcome data, risk factor data, and resource data.
Health Outcome Data
Outcome data are used to measure the presence or absence of health events (CDC, 1995). These data can be indicators of health status, and include death certificates and birth certificates that local health departments have issued. Such data can be used to evaluate the health of a local population, and they enable epidemiologists to look for clues as to the sources of particular health problems.
Risk Factor Data
According to Turnock (2009), risk factors include biological, environmental, lifestyle, and psychosocial elements, as well as the failure to use health-related services. These risk factors have been associated with diseases and certain adverse health outcomes. There is an enormous amount of secondary data available on the many factors that can predispose one to poor health. There are also ongoing epidemiological studies that provide new primary data on the extent of dangerous health practices.
Resource Data
Resource data inform communities of the health resources that are available to them for the prevention or treatment of disease. These include hospitals, physicians, clinics, and various other health care resources. Such data are very useful for public health planning purposes, including emergency preparedness.
Public health surveillance encompasses data collection for infectious and chronic diseases, injuries, environmental and occupational exposures, and personal behaviors that may contribute to the development of illness (CDC, 2009b). The techniques used in public health surveillance are not disease-specific, but can instead be applied to surveillance data concerning a variety of health conditions, exposures, and behaviors within a community. Public health surveillance is based on a very simple premise: understanding the problem is essential to solving it. Surveillance is the ongoing, systematic collection, analysis, and interpretation of health data integral to the planning, implementation, and evaluation of public health practice; it is closely integrated with the timely dissemination of these data to those who need to know.
Analysis of surveillance data often begins by summarizing them according to event or problem, person, place, and time. That is, it is a process of looking for patterns of disease or health outcomes among different groups, in different places, at different times. Identifying who got sick, where they went prior to and during illness, and when and for what duration they were sick yields valuable information about the types of disease control and prevention efforts that are needed and who should be targeted in order to most efficiently limit or prevent the spread of disease.
Looking for trends in surveillance data focused on health promotion and disease prevention behaviors is as important as focusing on the occurrences themselves. For example, knowing about patterns of vaccination coverage helps us understand why cases of vaccine-preventable diseases are declining, and patterns of caloric intake and physical inactivity help explain changing trends in the incidence of obesity and the subsequent increase in cases of type 2 diabetes.
The epidemiological concept of the triad of disease—agent, host, and environment—is extremely useful in explaining how diseases and injuries happen. It provides a starting point to begin viewing any health problem or issue. Researchers are now able to consider the reasons why a health problem might occur, and can move to a strategy focused on prevention rather than on finding a cure.
The process of surveillance starts with a statement of the health problem for which data are being gathered. The problem in question can relate to disease, injury, environmental contamination, or anything that researchers want to investigate. Problem statements have even been used successfully in solving marketing and management dilemmas. It is crucial to define the real problem, and not symptoms of a larger problem.
The second step in surveillance involves risk factor identification, or finding out the cause of the problem. The risk factor might be bacteria, a virus, secondhand cigarette smoke, obesity, or faulty machinery in the workplace. The techniques of epidemiology have given our country significant success in determining the cause or causes of many health problems.
The third step in the surveillance process is to find out what works to solve the problem under consideration. The best way to do this is to look at a number of potential solutions and conduct a cost-benefit analysis to find the one with the greatest chance of success at the lowest cost in terms of resource use. This step forces researchers to make a value judgment about various options for solving health problems while also considering the costs associated with their decision.
The final step in surveillance is the implementation of the system. Should it be an active or a passive surveillance system? A passive system would require researchers to alert the sources of their data, such as physicians and hospital laboratories, that they are interested in monitoring their data and are requesting their cooperation in the process. The assumption is that if these data sources see the data the researchers have requested, those researchers will be informed. Alternately, an active system would require researchers to alert the sources of data that they will be in contact at a prescribed time each week to ensure a timely reporting process. The active system works best when researchers are expecting the possibility of an epidemic, and this type of surveillance system is used every year during flu season.
Consider that in 1900 the leading killer was a communicable disease (tuberculosis), compared to 2010, when the leading killer was a disease often caused by avoidable health behaviors (heart disease). McGinnis and Foege (1993) took these data one step further and determined that the real causes of the disease are tobacco use, a poor diet, weight gain, and physical inactivity. With this revelation, the country was ready to use epidemiology to develop health promotion programs to educate people to prevent chronic diseases. It is interesting to note that life expectancy in 1900 was only forty-nine years of age, which has now increased by almost thirty years. This increase in life expectancy is not due to better medical care; it is the result of a better understanding of how disease occurs and how to prevent it. Thanks to this information concerning the real causes of disease, many in health care have started to look toward the idea of primary care that focuses on the prevention of illness and disease.
Epidemic Intelligence Service
The Epidemic Intelligence Service (EIS) is headquartered at the national Centers for Disease Control and Prevention. It is a two-year postgraduate program of service and instruction for physicians and other health professionals who are interested in receiving on-the-job training in epidemiology. After being trained in epidemiology, these medical officers are then assigned locations throughout the country for conducting epidemiological investigations, research, and public health surveillance. They are typically assigned to state health departments for a two-year assignment.
Epi-X
Epi-X is the CDC's Web-based communication system, which is available to most public health professionals. The system is used by CDC officials, state and local health departments, poison control centers, and other public health workers in order to communicate preliminary surveillance health information on a daily basis. Recipients of this information have been approved by the federal government, and have installed a secure certificate for their computer.
The Affordable Care Act passed by Congress and signed into law by President Obama in 2010 is in part an attempt to reduce health care costs by billions of dollars over the next several years. In order to attain these cost reductions, there is going to be a greater demand for efficiency from health care facilities and their managers. This will be accomplished through the use of comparative effectiveness research (CER), the findings from which will require better decision making by those in charge of health care delivery decisions. CER will subject many clinical procedures to rigorous evaluation to determine whether or not they are worth the cost, and if these procedures place the patient at unnecessary risk.
CER is one of the most promising parts of the new health care reform law, but it is going to change the way health care is delivered in this country. Nussbaum, Tirrell, Wechsler, and Randall (2010) point out that part of the new health care reform legislation includes an appropriation of $500 million more a year for the evaluation of medical services. This should reduce the costs of wasteful medical tests and procedures, producing $700 billion in annual savings every year. This process represents an attempt to control runaway health care costs through the elimination of waste, without reducing the quality of care.
CER represents an intense evaluation of different treatment options for a given medical condition. Weinstein and Skinner (2010) argue that CER offers a potential solution to the escalation in the costs of delivering health care in this country. What is more, the vast majority of countries that have reformed their health care system have included some form of CER in their final product (Mushlin and Ghomrawi, 2010). They have done so to protect patients from harm while attempting to simultaneously improve the quality of care and reduce health care costs. This law will produce an even greater demand for a new type of health care management.
This new emphasis an accountability in health care is an attempt to eliminate what has long been called “flat of the curve” medicine. This concept, made popular by economist Alain Enthoven (1978), suggests that as we continue to increase medical inputs in an episode of medical care, there will be successively smaller increases in medical output or value from the input. This does not imply that there is no benefit in completing additional medical tests and procedures, but that these additional inputs probably cost more than they are worth. They also may be dangerous for the individual, despite adding little if any value. Therefore, the concept of “flat of the curve” medicine underscores the need for vigorous evaluation of all inputs in the delivery of health care services. Public health program managers will bear this concept in mind when deciding how to eliminate the ever-growing list of threats to the public's health.
Looking to the science of epidemiology can offer managers of public health programs a better chance of success when making medical decisions and seeking to implement these effectively. Managerial epidemiology is a science to be practiced in the decision-making process concerning how best to make use of scarce health resources (Fleming, 2008). Managerial epidemiology can be highly useful, not only in gathering the requisite data to manage the outcomes associated with particular health care interventions but also in improving the functions of management that are most important for public health leaders and their program managers, including planning, finance, assessment of quality issues, and evidence-based public health practice.
Fleming (2008) argues that the planning function has a critical bearing on all of the management functions, and is by far one of the most important components of the changing health care system. Planning establishes the action steps that should be followed in order to achieve a successful outcome. Using the tools of managerial epidemiology should help those responsible for planning do a much better job at gathering the data necessary for making thoughtful decisions about how to distribute scarce resources. Managers could, for example, explore the descriptive epidemiological data in order to better frame the problems their agency encounters. They could then use the tools of analytical epidemiology to look for statistical relationships among the various data sets. This will allow more accurate predictions of outcomes resulting from medical interventions. A very good example of the use of managerial epidemiology is found in the development, implementation, and evaluation of community health planning found in the series of Healthy People reports, completed by the Department of Health and Human Services, each of which was developed and used for a ten-year time period.
It is obvious that managerial epidemiology can help leaders and managers work with the guidelines and procedures of evidence-based public health practice. This will enable public health departments to use epidemiological techniques in evaluating their interventions and sharing the success stories with other community health facilities. In fact, managerial epidemiology will allow these departments to continually develop and share best practices in disease prevention efforts with the entire health care system. This allows the application of evidence derived from observational and experimental studies to medical decision making.
Fleming (2008) argues that preventive medicine is not practiced as often as necessary in order to improve population health, probably because of the lack of appropriate information systems. Managerial epidemiology may very well be the missing component required to bring evidence-based preventive medicine into widespread use among the majority of individuals who work in health care and who have responsibility for the use of scarce health care resources. Health reform efforts that include the expansion of proven preventive programs may have the ability to reduce health care costs while maintaining the quality of health care delivery.
Application of Epidemiological Concepts to Health Care
The health care system is well on its way to developing best practices that will be part of an overall shift toward evidence-based approaches in medicine and public health. The tools of epidemiology can be extremely powerful in helping reform the way health care is delivered in the United States. Sophisticated surveillance systems, community assessment techniques, descriptive epidemiology, analytical epidemiology, and managerial epidemiology are scientific concepts that public health departments must share with the rest of the health care system.
There is very little disagreement that there is tremendous waste in our current health care system. So the question has become, How do we determine what should and should not be done in health care? This is where the science of epidemiology comes into play, by helping decision makers gather and evaluate all of the available outcome data that are so necessary when making decisions that involve population health. This is a movement away from operating on hunches about causation of disease toward seeking more precise definitions of causation.
According to Lee and Mongan (2009), in order to bring health care costs under control, the diffusion of the development of new health technology must be slowed. We must be able to determine the costs and benefits of new technology tools, which has always been a serious challenge for providers of health care services. This is where epidemiologists can help decision makers understand costly changes before they are incorporated into medical practice. This is of particular importance because once these technology tools become part of health care delivery, they are very difficult, if not impossible, to control.
Christensen, Grossman, and Hwang (2009) argue that it takes disruptive innovation to change the way we deliver goods or services. Disruptive innovation entails a process through which complicated and very expensive products or services become simplified and less expensive. This happens when innovation and creativity become incentivized in the business model; and this concept would certainly apply to the delivery of health care in this country.
Now let's apply the concept of disruptive innovation to improving the health of the population at a cost that we can afford. In order to be successful in this venture, we need to develop and apply a model of health care that is different from the one we have been using. We must apply the idea of disruptive innovation to the delivery of good health to the U.S. population, not just to individuals.
In their new book titled The Innovator's Prescription: A Disruptive Solution for Health Care, Christensen, Grossman, and Hwang (2009) assert that health care is attempting to move from an intuitive to a precision approach. They define intuitive medicine as a craft that deals only with symptoms and a treatment for the symptoms that is uncertain. Precision medicine, however, focuses on precise diagnosis of a disease, which is then treated with proven therapy. This is where the science of epidemiology can serve us well by providing statistical data that show the real causes of many medical conditions.
The way that the health care system in our country is structured, especially in regard to how we reimburse providers, means that it is incapable of sustaining innovation. Therefore, we need the same type of disruptive innovation found in the business world to move the health care system away from a preoccupation with curing disease and toward disease prevention. At the same time, public health departments must shift their focus from the control of disease to the prevention of disease.
In order for disruptive innovation in health care to prosper and grow, we have to change the way we pay providers for the delivery of medical services. The current payment system offers incentives for more care, which allows illness to occur and discourages providers of care from spending time on prevention efforts.
What is more, this same type of disruptive innovation has to become the norm in the delivery of public health programs. Just as the science of epidemiology can be a necessary adjunct to the development of precision medicine, a better understanding of epidemiology allows public health departments to change their emphasis on communicable diseases to a stronger focus on the causes and prevention of chronic diseases. Epidemiology can become the catalyst of disruptive innovation to help reduce the costs associated with the development of chronic diseases and their complications.
Epidemiology is one of the great assets of public health, and should be essential in dealing with the health care crisis. Decision makers who are responsible for the distribution of resources in health care delivery have to understand and use epidemiological principles. Several of the tools that are available to the epidemiologist can also be helpful to medical care professionals who must decide how to bring costs down and improve the outcomes associated with various medical procedures.
The increase in life expectancy since 1900 is not because of better medical care, but rather due in large part to a better understanding of how disease occurs and how to prevent it. By learning the real causes of disease, physicians have started to shift away from the concept of curing disease and toward the idea of primary care that focuses on disease and illness prevention. Epidemiology is a science that can assist health care professionals in making informed decisions about how to use scarce resources; it can also facilitate the gathering of the requisite data to help better manage the outcomes associated with particular health care interventions. What is more, epidemiology is also useful in the improvement of the major functions of public health management, including planning, finance, assessing quality issues, and evidence-based public health practice.
Analytical epidemiology
Case definition
Chain of infection
Descriptive epidemiology
Direct transmission
Epidemiology
Indirect transmission
Managerial epidemiology
Triad of disease
1. Explain the use of epidemiology in many of the successes public health departments have achieved over the last one hundred years.
2. What are some of the major differences between descriptive and analytical epidemiology?
3. Offer a thorough explanation of managerial epidemiology. How can this concept be used in making better decisions concerning the allocation of scarce health resources?
4. How can the principles of epidemiology be applied to the process of innovation to solve the problems of cost and quality in our current health care system?