5
NURSING ROLES IN THE IMPLEMENTATION OF CLINICAL INFORMATION SYSTEMS
Contents
System Implementation: The Design Phase
System Implementation: Go-Live
An electronic health record (EHR) is a standardized, efficient, and accessible way to provide information to clinical staff across the continuum of care. A clinical information system (CIS) is the foundation of the EHR. Most healthcare institutions have embraced the 1999 Institute of Medicine report To Err Is Human: Building a Safer Health System. This study identified that faulty systems or processes most commonly cause errors.1 Follow-up studies from the IOM, Crossing the Quality Chasm2 and Keeping Patients Safe: Transforming the Work Environment of Nurses,3 address the role systems play in safe, quality care. Driving forces for CIS implementations include clear documentation, real-time access, timely execution of orders, and quality care consistent with best practice.4 Successful implementation relies on identifying key clinical champions and defining their specific role in the implementation. While all clinical stakeholders are important to the implementation, nurses can play a unique role in each phase, and at every level, of the implementation. Including nurses in the selection, design, and implementation teams and giving them a significant role is one key to a successful implementation. Nurses can facilitate end-user engagement, enhance system design, provide education, sponsor change management, and effectively communicate to all other stakeholders. Because their focus is patient-centered care, they can support most clinical disciplines where tapping into this pool of experts is a recognized way to successful implementation.
Implementation Roles
There are many roles in a CIS implementation. Different levels of experience are needed and responsibilities vary for each role. As system implementation has many phases and each phase requires different knowledge and skills, the roles and responsibilities vary at each phase. The phases include system selection, design and go-live, and system optimization. Implementation roles include executive sponsor, project director, team leader, clinical system analyst, educator, and superuser.
One important team in the process is the executive steering committee, which assumes responsibility for the project, ensuring that the vision is identified and communicated, and escalated issues are resolved. The committee members provide top-down, visible support to the team members. Very often the chief nursing officer (CNO) and the chief information officer (CIO) co-chair this committee, and additional members attending this committee include the chief financial officer (CFO), chief medical officer (CMO), chief medical informatics officer (CMIO), and department chairs. The executive steering committee will resolve any issue that cannot be resolved by the project teams, where typically these issues relate to resources or budgeting concerns.5 During the course of the project, the teams may need additional resources because some steps in the project plan may take longer than anticipated to complete. In addition, the team may uncover a more complicated process that could delay the go-live date. These issues will be resolved by the executive steering committee, led by the executive sponsor.
Executive Sponsor
Deciding who will be the executive sponsor is a critical step in the implementation. The CIO oversees the entire project, and the role of executive sponsor is one that bridges the gap between the technical and the clinical environments. The person in this role ensures that the clinicians are fully engaged in the implementation. The executive sponsor will help align system design with clinical outcomes and will establish implementation goals that will support the organization’s mission, vision, and values. The sponsor will also determine strategic and business objectives, communicate the vision to stakeholders,6 and help define the scope of the project, ensuring that mission-critical applications are given highest priority. Finally, the executive sponsor reports project progress to senior leadership and to the board of governors.
Project Director
The project director is responsible for overseeing all of the teams associated with the implementation. These teams will be application specific and can include such areas as clinical documentation, order entry, pharmacy, or radiology. Each team will have its own project plan with tasks and milestones that are specific to the application. There will also be some items, such as selecting point of care devices, system security, and printing options, on each of the plans that are common to all of the applications. The project director must be able to coordinate multiple project plans and ensure that milestones in the plans are met. Each of these plans must be synchronized across all applications so that common milestones are addressed once for all teams. Each of these plans will roll up to the main project plan for the entire implementation, where the responsibility of the project director is to ensure that the project milestones are met.
The project director must have the respect of end users as well as administrators, as they align the organizational goals to the project goals. This individual is generally a person who is comfortable with both the technical and clinical aspects of the system. The director will develop the project plan and direct every aspect of the project,7 where his or her responsibility is to ensure that the team is meeting the project goals and following the project plan, which includes resolving issues within or across applications. Meeting project milestones, identifying regulatory changes that will affect the design, and monitoring the budget are key components of project direction, and the director ensures that an effective change management strategy is in place. While the executive sponsor will identify and communicate vision, it is up to the director to manage the teams and keep the vision aligned at all aspects of the project plan. Finally, the project director should be an active member of the project steering committee, reporting on project progress, team accomplishments, and issues, and will work with the vendor to manage the project timeline.
Team Leader
As there may be multiple applications and multiple teams in the implementation process, an additional role to be filled is that of team leader. This person fills the role of managing one application, or team; provides oversight to the individual application team; keeps the team members on vision and team goals aligned with the vision, and matches resources to each task.7 The team leader generally reports to the project director and is responsible for the daily operations of the members of the application team. The team leader is generally well versed in departmental operations and has detailed knowledge of the application and can apply both a technical and a clinical focus to it. Part of his or her task is to assign a clinical system analyst to project tasks, ensuring the analyst has the competence to complete the assignment. The team leader will also coordinate with the other team leaders on duplicate tasks across the entire project, chair team meetings, provide updates to the project director, and resolve individual issues within the application and escalate to the project director those that cannot be resolved.
Clinical System Analyst
The application team is responsible for bringing the finished product to end users8 and completing the tasks associated with the application project plan. Working together are representatives of all disciplines, including nursing, physical therapy, dietary, respiratory therapy, medical records, and finance. Members can be either permanent or ad hoc team members, where the permanent members of this team are called clinical systems analysts (CSAs).
The CSA reports to the team leader and focuses on workflow analysis, software requirements, and design of the application to meet organizational specifications.6 The CSA conducts an assessment of existing workflow and the current operational process and receives education on the system from the vendor. The education will provide the CSA with knowledge of system functionality and how to design the system, where on completion, the analyst will be the expert on the application. In collaboration with clinical staff, the analyst will evaluate how the system can be adapted to meet clinical outcomes and departmental and organizational goals. The department manager, in collaboration with the project director, will identify resources for the evaluation, and the CSA will work with these resources, who will be experts on the current operational process.
Educator
New system implementation requires competent users. To ensure this, end users will need formal education to develop the skills to use the system because no matter how well designed the system is, if the end user does not learn the system, the implementation will fail. The educator will determine when training will be conducted,5 and the project director, in collaboration with the executive sponsor, will identify the additional trainers, class location, and logistics. The selection of the staff to train end users will depend on the applications to be implemented, and the educator will have a detailed knowledge of how the system works and the operational process of the end users.
The project director and the educator will develop the education plan that determines logistics, such as number of educators, appropriate class size, process for scheduling end users, and identification of clerical support services. The educator will be responsible for development of lesson content, the process to measure competency, and skills validation. The lesson content will include both application procedures and workflow redesign, and the educational session will be concept based rather than task oriented. Ultimately, the emphasis will be on integrating technology and workflow.
Superuser
Another important member of the team is called a superuser. Superusers are peers who will help train and support their colleagues in the implementation process.9 They are active members of the implementation team and will provide input into the design of the system. Superusers generally possess excellent communication skills, expert knowledge of department operations, and are coaches to their peers. The superuser, as nurse champion, facilitates communication in two directions: articulating nursing needs to the CSA and explaining technology solutions to the nursing staff.10 Superusers help decrease dependence on the CSA, are a department-based resource, and have expert skills in the use of clinical applications.11 The superuser should be flexible and understand the internal chain of command for resolution of issues. Additionally, he or she will provide input into policy revision and procedure redesign. The CSA will follow superusers through their workday and log each of the steps and document each task and how the task is completed. This will provide the basis for documentation of the current workflow. The CSA compares the current workflow and applies it to the design of the system, where the superuser offers guidelines for documentation, participates in system selection, completes system testing, and trains and supports his or her colleagues.12
The Phases of Implementation
Once the implementation roles are defined for the institution, it is up to the executive team to match the appropriate clinician to the role. Each role actively participates in all phases of the implementation. Nurses should have a prominent role as champions on the implementation team given their professional experience and knowledge.10 Nursing roles include the CNO, informatics nurse specialist, nurse educator, and staff nurse. Involving nurses in education, go-live support, and system optimization is one of the key factors to success.13 This concept is supported by a study that concludes that successful implementations are ones that are owned, sponsored, and championed oned by the nursing team.13
There are several phases in the life cycle of an informatics project: selection; implementation, which includes design and go-live; and postimplementation system optimization. In the selection phase, the focus is finding the right system for the institution. In the design phase, technology and workflow will be integrated to facilitate best practice, and in the go-live phase, support for new users of the system will be the priority. System optimization prepares the clinicians for less intense activities of maintenance and enhancements, where they will eventually fully own the system, with the project team transitioning to a supporting role.
System Selection
In the role of executive sponsor, the CNO has a strategic position in system selection. In collaboration with the CIO, CMO, CFO, and CEO, the CNO identifies and communicates the organizational vision for management of information.14
The CNO will be actively involved in selection and implementation of information systems, a policy that is supported by The Joint Commission (TJC), which requires nursing involvement in the selection process.15
The executive steering committee determines the budget for the project, identifies the participating disciplines, and approves the standards by which vendors will be evaluated. The committee will ensure that organizational goals are congruent with the system and evaluate the vendors from a macro perspective. By networking with their peers, the committee will be able to compare vendor solutions for systems that are functioning at similar institutions. The executive team will also approve the request for information (RFI) and request for proposal (RFP) documents. Members include administrators from nursing, medicine, pharmacy, information technology, operations, and finance.
Ideally, a nurse with clinical, informatics, and implementation experience is an ideal candidate for the role of project director given his or her broad background across a variety of processes in the healthcare spectrum. An informatics nurse specialist is a nurse who is formally trained in the practice of informatics. This involves the management and utilization of information and technologies. Responsibilities for this role include development of systems, research to support information systems, and making information systems usable for nurses.16 The informatics nurse synthesizes informatics standards into every aspect of the implementation. With an American Nurses Credentialing Center (ANCC) certification in nursing informatics, project management certification, or as a Certified Professional in Healthcare Information and Management Systems (CPHIMS), the project director will have the knowledge and skills necessary for this role. The ability to follow a plan, identify barriers, and resolve issues is a common skill in nursing practice. The director has experience in managing multiple patient priorities that enables him or her to manage multiple application project priorities.
The project director completes the RFI and RFP documents. The director, in collaboration with directors from other disciplines, will identify requirements from a technical and clinical perspective, where functional requirements are included in these documents. He or she will also include information about the institution, such as number of beds, facility structure, annual admissions, and annual outpatient visits. This will allow the vendors to better prepare a proposal. Those vendors who cannot meet basic functionality are eliminated from the selection process.
Evaluation of the systems that make the first cut will give an end-user view of how the systems function in day-to-day operations. This will allow the selection team to further narrow down the field of systems. The final evaluation will ensure that patient-centered care is maintained through electronic documentation, improved accuracy of documentation, and clinical decision support.15 The project director completes a functional needs assessment that details the necessary functions a system should have. The functions will be based on regulations, policy, and best practice. The director will then develop the assessment listing the key components for the system, specific to the institution, that identifies the “must haves” for the system (Table 5.1). For example, does the system allow standard tables/drop-downs across modules? The director will determine if this is a requirement or an option. Each system is evaluated by the functions, and a decision is made once all system evaluations are complete. The functional assessment is combined with other factors, such as cost and technical requirements, to identify the top choices. The next step is to identify the team to see the top choices in action. The director will coordinate the site visits and ensure that all disciplines are represented on the visit. Once the site visits are complete, and the assessments are made, the director will prepare a recommendation to the executive team.
Table 5.1 Example of a Functional Assessment for Clinical Documentation
| SYSTEM FUNCTIONALITY—CLINICAL DOCUMENTATION | PRESENT YES/NO | REQUIRED YES/NO | DESCRIPTION/ COMMENTS |
|---|---|---|---|
| Does the system allow standard tables/drop-down menus across modules? | |||
| Can documented information be pulled from encounter to encounter? | |||
| Can documentation in all encounters update information in history? | |||
| Does the system support multidisciplinary documentation? | |||
| Are problem lists supported? | |||
| Can documentation generate a charge to the financial system? | |||
| Can documentation generate acuity? | |||
| Can alerts be generated based upon documented fields? | |||
| Can sets of information be required? | |||
| Can documentation be set up to specific patient populations? | |||
| Can documentation trigger orders? | |||
| Can documented problems generate orders or interventions? | |||
| Can problems be prioritized? | |||
| Can the system prevent future documentation? | |||
| Are there templates for progress notes, op notes, etc.? |
The next step in the selection process involves the staff nurse and front-line direct caregivers. This is when the top vendors will come to the institution to demonstrate their system. Te staff nurse as superuser can be a valuable asset at this stage. The team will want to see how the systems work in their own environment. Staff nurses will help prepare a script of the typical patient encounter at the institution. The systems should be evaluated across the patient care continuum and include the most common patient populations. The best way to accomplish this is to use the system to follow the patient experience through orders, documentation, and follow-up care. Enabling direct caregivers to walk through the system will provide an opportunity to “test drive” it. Designated staff nurses will become engaged in the selection process, where they will be the early adopters and help create a pool of superusers who will assist through the next steps of the implementation. Once the site visits and demonstrations are complete, the selection team will complete evaluations of each of the vendors and the director will compile the results and make a recommendation to the executive committee.
At this point, contract negotiations will be held. The project director will evaluate the contract for inclusion of requirements identified in the functional assessment. The chief counsel, CIO, CNE, and CFO will complete the negotiation team, and they will have the final decision and take all aspects of the selection steps into consideration. The signing of the contract will start the next phase, system implementation. See Figure 5.1 for a stepwise illustration of the entire process.

Figure 5.1 The steps of the system selection.
System Implementation: The Design Phase
After the contract is signed, the executive steering committee identifies the team for the implementation phase. The executive sponsors’ primary responsibility is to facilitate end-user engagement in the design. The executive steering committee team will determine the scope of the project and identify which applications will be implemented first. The implementation team members will be assigned to each application based on their clinical expertise. The application team will assess the needs of the end users, and a formal needs assessment will capture their basic requirements for system functionality. The assessment will include collecting information needs, workflow process, and functional requirements, where the requirements indicate what must, must not, may, or should be included in the design of the system.17
The team should meet frequently with the superusers in this phase, during which the CSA designs the system and provides feedback on the design to the superusers. As executive sponsor, the CNO focuses on the administrative aspect of the design, keeping in mind the strategic goals, mission, vision, and values, making certain that the best candidate is assigned to the role of the project director.
Much of the high-level implementation activity is the responsibility of the project director. The director applies project management and informatics standards, integrating nursing science, computer science, and information science. Project activities include analyzing, testing, and implementing systems to support patient care. The project director will have communication, change management, and business and application knowledge,16 and the director will guide the application teams through the steps of system design.
The director is also responsible for multiple teams and multiple applications. The scope of the project will determine the required skills of each CSA and the number of analysts needed per application. If the implementation consists of many applications, team leaders will be assigned to each application. The director ensures that the project plan is developed and that the team stays on track for the expected go-live date. Key milestones and target dates will be identified, and it will be the responsibility of the project director to keep the team on target. Ultimately, the CSA will follow the plan and complete the tasks in the application plan.
Success in system implementation will depend on the nurse having a prominent role in change management, with nurse champions on the team.10 The CSA will review basic system functionality and match it to the clinician workflow, and will identify and review all departmental policies and procedures that relate to the implementation. He or she will evaluate the screens provided in the basic system and tailor them to end-user specifications. The CSA also collaborates with superusers to identify and incorporate best practices into the system, where system design should include standard terminology and required minimum data. Required data are the essential information that must be included for completion of the process. In this case, the user cannot leave a computer screen without entering the information. This guarantees that minimum data are collected.
The nurse in the CSA role documents the current operational workflow associated with the application, which takes place over several days in various ways. Workflow process analysis leads to a clearly defined diagram of how tasks are completed by the clinical staff. This step requires frequent interaction with the clinicians. These interactions include a formal interview to detail the step-by-step process needed to complete the task. Time to shadow the clinician is also necessary to verify the accuracy of the documented process. Superusers comfortable with the current documentation process will be the primary resources for documentation of workflow, where several episodes of shadowing are necessary. The CSA will follow the superusers through their workday and keep a log of the steps documenting what they do and how they do it, and complete the diagram of current process. The goal is to integrate the current best practice, new functionality, and technology into one seamless process.
Workflows will be created for each of the operational processes associated with the functions in each application. For nursing work-flows, this will include the medication administration process, documentation of patient assessments, vital signs, intake and output, and care planning, where all details will be included. As each workflow is documented, the appropriate administrator will sign off to validate the accuracy of the documented workflow. The CSA will then compare the current process to the functionality in the system and will also take into consideration any new point of care devices or steps that will be added to the workflow at implementation. A proposed new workflow will be diagramed to show how the new system will change the process.
Figure 5.2 shows a typical new medication management workflow for a physician, pharmacist, and nurse after implementation of the CIS. The new process will build safety into each step with the addition of computerized physician order entry (CPOE), clinical decision support system (CDSS), point of care (POC) technology, and bar-coding for medication administration (BCMA). Automated dispensing cabinets will improve turnaround time and provide another level of safety. For physicians, CPOE with CDSS will provide patient-specific recommendations to assist in making clinical decisions.2 For nursing, it is important in this phase to recognize the implementation as practice redesign. Current processes and workflows will change in order to implement a new evidence-based practice model.13
The CSA designs the system based on the details in the new work-flow. After completing the screen builds, data entry fields, and tables, the CSA compares the current process to the proposed new process, where the comparison of the two workflows will generate an impact analysis. The executive sponsor and appropriate department leaders then review and sign off on the new process and the impact analysis, which will be used to prepare the end users for the new system. It will form the key items to stress in education for the end users. The superuser will communicate the new process prior to formal education to better prepare the end users for the change, and will champion the new workflow as one that is beneficial to delivering patient care.11 Holding regularly scheduled sessions with the superusers will provide them with the information to validate and communicate the change. Figure 5.3 shows the process for identifying and detailing the current process, proposed new process, and impact analysis.
On completion of the new workflows and revisions to the system, the CSA will start the testing phase and complete individual testing within each application. This will verify that the application build works as intended. Then the CSA will test across applications, where once the verification at this level is complete, the superusers will test for usability and accuracy. Testing should be integrated to include hardware, interfaces to ancillary systems, and the billing process. Testing new point of care devices will identify any network issues, and if the network is unreliable, the devices will not consistently be available for the end user.18 Superusers from all disciplines will participate in the final level of testing, and they will sign off on the work-flow and screens. The project director then confirms all is ready to start training the end users.
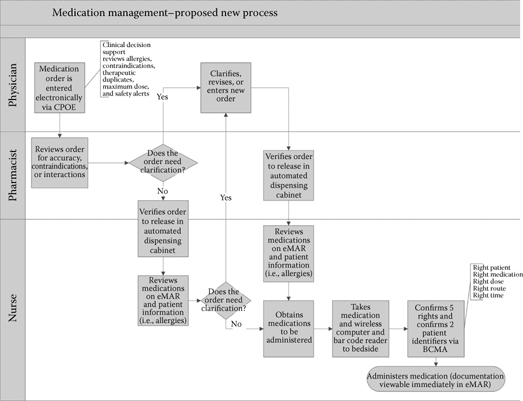
Figure 5.2 Medication management proposed new process for CIS implementation.

Figure 5.3 Process for current, proposed, and impact workflows.
Ideally, classes should start shortly before the staff is scheduled to begin using the system. Planning too far ahead may result in users forgetting what they were taught.5 Together, the project director and the educator will develop the education plan. It should be kept in mind that classes should be scheduled at times that are convenient for the end users. This will require a large pool of educators who can conduct classes on all shifts, seven days a week. Managers will be responsible for maintaining minimum staffing levels on their units while sending staff to class, and the educator will select and train the class instructors. Super-users are generally excellent choices for instructors given their expert knowledge of the new workflows and the system. The educator will monitor class attendance to ensure the majority of users are educated prior to go-live, and completion of class will be mandatory prior to granting access to the system. Each attendee will be expected to demonstrate competency by completing a test on the new workflows and system, where once education is complete, the end users are ready to use the system. Figure 5.4 shows the process for the steps up to go-live, including education and issue resolution.

Figure 5.4 Steps in go-live phase of implementation.
System Implementation: Go-Live
The go-live is the date on which the staff will begin using the new system. The date is one set by the executive team from the recommendation of the project director. Consideration for the decision includes availability of resources to support the go-live and organizational initiatives that could divert resources or attention from the go-live. At this point, education of end users must be complete and the system must have passed integrated testing.
The executive sponsor and project director must be sure that the support for go-live is adequate. Whether the go-live is a pilot on one unit or whole house, users must be adequately supported. This implies that requests for assistance must be responded to in real time and the entire implementation team will be available to support all users. The superuser will provide on-unit support for basic troubleshooting and resolution of operational issues5 and will triage more complex issues to the support team stationed in a go-live command center.
During the go-live period, a log should be kept of all calls to the support team. The information that will be logged includes name and location of the caller, description of the issue, category of issue, responsible party, and resolution of the issue. The issues will be identified into three categories: operational, technical, or educational, where the category of the issue will determine who will be the responsible party to resolve. The issue log will provide a mechanism for trending analysis and will help the team to determine if they are isolated events or part of a more global problem. The log should be posted for all end users to view, which will allow them to see the response and to reach out to the responsible party with any questions. In the case of educational or operational issues, it can also help prevent the issue from occurring again by another user.
The support team located in the command center will be a combination of vendor support staff, CSA, team leaders, and the project director. Additional support will take the form of a roaming team of superusers on the units to resolve operational and educational issues. Support will be 24/7 and will remain in place for as long as calls are coming into the command center. The number of staff needed for support will decrease after the first week, and then the team should be able to transition the support to the superusers and normal support staff. The transition from active 24/7 support to standard support operations will be determined by the CIO, executive sponsor, and project director. Nursing administration will take the lead in establishing a team for ongoing operational support for the end users, where this support team will answer questions about documentation, provide advice on how to improve new workflows, and continue to log and trend issues. The post-go-live superusers will be well versed in the CIS and new processes.19
The executive sponsor and the members of the executive steering committee should have a visible presence during the go-live, in the command center and on the units. The executive sponsor and project director’s responsibilities are to ensure that the transition for the front-line staff is seamless. The executive sponsor will empower the clinicians to take ownership of the system and the new process. Finally, the CNO should understand the impact of the implementation on all levels of the organization.15
System Optimization
Following the go-live period, the project team will begin the optimization phase, at which time they will evaluate enhancements to be implemented. These enhancements may be suggestions or noncritical issues from the issue log. They could also be items that were deferred during system design due to time constraints. The project director will prioritize the enhancements and the team leaders will implement the solutions.
The executive sponsor and the project director will determine the metrics by which the implementation will be measured. Some of the critical success factors include staff satisfaction, patient satisfaction, increased time at the bedside for the nurse, increased accuracy in documentation, the timeliness of information, and the accessibility of information. The pharmacy and pathology areas will measure turnaround time, number of clarifications, and number of prevented errors by clinical decision support alerts.
Staff satisfaction should improve with the implementation of more efficient and effective workflows. To measure this, a satisfaction survey should be conducted after some time has elapsed following the system rollout. Typical questions in this survey include ease of documentation, speed of response by the support team, and turnaround time for recommended changes.
Another way to evaluate success is to monitor the quality and completeness of documentation, where the minimum required data identified in the planning stage could be used as indicators for performance monitoring. Accuracy and completeness should be key elements considered. The evaluation should be simple since computerized data are more accessible and retrievable than handwritten documentation. Other evaluations should then be completed based on quality of documentation, assessment of national patient safety goals (NPSGs), TJC standards, and organizational policy. Completion of documentation, such as assessment and reassessment of pain, within specified time frames can be measured.
The executive steering committee will prioritize and allocate resources for monitoring the effect of implementation on the clinical workflow and patient outcomes. The implementation will also streamline and automate the process for reporting of public data. The team can use the driving forces for the implementation to assess their performance.4 See Figure 5.5 for a stepwise illustration of the process.
Conclusion
The implementation of a CIS is a process that requires teamwork. Assembling the best teams will ensure a successful transition to new workflows, automated processes, and real-time clinical decision support, where the teams must represent all disciplines. The inclusion of nurses at all phases and in key roles of the implementation will help ensure for end users that the implementation will be patient centered. The selection phase will allow the team to see the systems in action being used by their peers. The design phase is the best opportunity to get buy-in from nurses and other disciplines, which includes understanding the current process and integrating technology into best practices to redesign clinician workflow. Education is a very important consideration in this phase.

Figure 5.5 Post-go-live processes for system optimization.
To achieve a smooth go-live rollout, dedicated staff support by the implementation team is necessary. The team, in collaboration with administration, will decide the day the clinicians begin to use the new system, where well-trained and supported users should begin to utilize the new platform. In the optimization phase, the team will evaluate the implementation, where feedback will include a staff satisfaction survey. The team will monitor documentation for accuracy and completeness.
Implementation of a CIS should ultimately increase accessibility and improve the accuracy of documentation. In the end, an implementation is costly, time- consuming, and resource-intensive, but the return on investment should be worthwhile given the positive impact on clinical outcomes. Including new technology in the redesigned workflow will improve safety with real-time clinical decision support, improve quality with more complete documentation, and improve satisfaction by increasing nurse time at the bedside. Having nurses in key implementation roles will ensure that the patient is the primary focus of the implementation.
This chapter was originally published in Healthcare Informatics, Improving Efficiency and Productivity, Taylor & Francis, New York, 2010.
References
1. Kohn LT, Corrigan JM, Donaldson MS, eds. 1999. To err is human: Building a safer health system. Washington, DC: Institute of Medicine Committee on Quality of Health Care in America, National Academies Press.
2. Institute of Medicine Committee. 2001. Crossing the quality chasm_ A new health system for the 21st century. Washington, DC: National Academies Press.
3. Page A, ed. 2003. Keeping patients safe: Transforming the work environment of nurses. Washington, DC: Institute of Medicine Committee on the Work Environment for Nurses and Patient Safety, National Academies Press.
4. Mustain JM, Lowry LW, Wilhoit KW. 2008. Change readiness assessment for conversion to electronic medical records. JONA 38:379–385.
5. Maffeo R. 2000. Project implementation: A tailored approach. Semin Nurse Managers 8:51–52.
6. Hassett M. 2006. Case study: Factors in defining the nurse informatics specialist role. Jhim 20:30–35.
7. Staggers N. 1998. Notes from a clinical information system project manager: Requisite survival skills. Comput Nurs 16:244–246.
8. Souther E. 2001. Implementation of the electronic medical record: The team approach. Comput Nurs 19:47–55.
9. Ball MJ., Hannah KJ, Edwards MJA. 1999. Introduction to nursing informatics. New York: Springer-Verlag.
10. Kirkley D. 2004. Not whether, but when. JONA 34:55–58.
11. Boffa DP, Pawola LM. 2006. Identification and conceptualization of nurse super users JIHM 20:60–68.
12. McNeive JE. 2009. Super users have great value in your organization. Comput Inform Nurs May/June: 136–139.
13. Murphy J. 2009. The best IT project is not an IT project. JIHM 23:6–8.
14. Brokel J. 2007. Creating sustainability of clinical information systems. JONA 37:10–13.
15. Simpson RL. 2007. The politics of information technology. Nurs Admin Q 31:354–358.
16. American Nurses Association. 2008. Nursing informatics: Scope and standards of practice. Washington, DC: American Nurses Publishing.
17. Brady M, Hassett M, eds. 2000. Clinical informatics. HIMSS Guidebook Series. Chicago: Healthcare Information Management and Systems Society.
18. Huvane K. 2008. Trouble at the bedside. Healthcare Inform 25:32–35.
19. Shedenhelm HJ, Hernke DA, Gusa DA, Twedell DM. 2008. EMR implementation and ongoing education. Nurs Manage July, 51–53.
