Coping with Uncertainty. Resilient Decisions in Anaesthesia
This study aims to describe the variability anaesthesiologists deal with in their everyday work and to understand the different strategies used by them to avoid the negative consequences of this variability. An empirical research, based on the critical-incident technique was conducted in a paediatric anaesthesiology service in a French hospital. The results highlight a distinction between potential situations in which the problem was envisioned beforehand by practitioners and unthought-of situations which were unthinkable for the anaesthesiologist previously and at the time of their occurrence. This subjective classification based on ‘the astonishment of the perceiver’ highlights two critical decisions made by anaesthesiologists in order to manage variability. The first is the preoperative definition of an envelope of potential variability of the surgical intervention. The second concerns the occurrence of an event which trespasses the envelope initially defined and requires the mobilization of additional resources. The identification of these two critical decisions provides opportunities for researches and actions to enhance resilience in the practice of anaesthesia.
States of Resilience and Uncertain Events
Resilience is the intrinsic ability of a system to adjust its functioning so that it can sustain required operations under both expected and unexpected conditions. This latter definition proposed by Hollnagel (Prologue of this book) emphasises the breadth of the concept, indicating that resilience is not only the system’s ability to cope with unforeseen variability that fall outside the expected areas of adaptations (Woods, 2006a) but also looks at its ability to operate in foreseen conditions. Indeed, since the appearance of the term resilience in the field of safety, many models have attempted to characterise the systems’ domains of variability, in order to clarify this ability (or these abilities) to be resilient. These models generally cut ‘the space of possibilities’ according to the frequency of the disturbances that a system or an organisation may be facing. Indeed, a system that is resilient when a regular threat occurred will not necessarily be resilient facing an irregular threat or an unexampled event (Westrum, 2006). Thus, states of resilience can be defined as those proposed by Hollnagel and Sundström (2006): the state of normal functioning, the state of reduced irregular functioning and the state of disturbed functioning. A resilient system is then one capable of detecting that the conditions have changed, to assure transition to another state and to operate in the new state of resilience achieved.
Other studies have modelled how systems make adjustments to address these different types of uncertain disturbances, notably by describing how these systems behave when they must operate under high pressure. By analogy to the physical model of materials ‘stress and strain’, Woods and Wreathall (2008) distinguish two adaptation areas.
1. The uniform or elastic region, in which the organisational response is proportional to the increasing stress. In this region, there are plans, procedures, training and resources provided to allow the system to adjust to demand. This area corresponds to the envelope for which the system is designed (Woods, 2006a).
2. The non-uniform or extra region, for which the organisation’s responses can no longer proportionally cope with the increasing load: failures appear and performance deteriorates (Wears et al., 2008). In this region, additional resources are mobilised and local strategies are deployed by individuals and teams to deal with disturbances.
Similarly, based on the model of socio-technical systems proposed by Rasmussen (1997), Miller and Xiao (2007) describe two adaptation areas: the compensation area (that corresponds to the marginal zone of the Rasmussen’s model) and the decompensation area. The marginal zone represents ‘the system’s ability to cope’ (Rasmussen, 1997). In this area, ‘opportunistic processes’ outweigh the disruptions: a range of behaviours and resources are mobilised to maintain the operating system to a level of risk as small as possible. Such compensations can sometimes mask the presence and the development of dysfunction (Woods and Cook, 2006). Once the compensation mechanisms are exhausted, the system decompensates: parameters suddenly collapse and potential for failures increases. This decompensation may be chronic or acute (Miller and Xiao, 2007), or both at once (Wears et al., 2006). Therefore, the study of resilience requires describing these different classes of adaptive processes that allow a system to adjust its functioning so that it can pursue operation under varying conditions (Woods and Cook, 2006).
Describing How Anaesthesiologists Manage Uncertainty
In the context of research on patient safety in paediatric anaesthesia, we sought to describe the variability that anaesthesiologists deal with in their everyday work and to understand the different strategies used by them to avoid the negative consequences of this variability. Indeed, with a risk of a fatal accident less than 1 per 100.000, anaesthesia is now faced with the ‘paradoxes of safe systems’: to continue to progress on safety, it is necessary to change the nature of the system and to consider different safety measures (Amalberti, 2001; Amalberti et al., 2005). One way could be to envisage specific training methods, similar to those used in the aviation domain with simulators (cf., Chapter 8). The objective of this study is then dual: first, it seeks to identify the different types of disturbances that anaesthesiologists have to manage in their real work activity and, second, to highlight the resilience factors, that is, the strategies developed in practice by anaesthesiologists to allow the system to function despite these disturbances.
The study was conducted in a paediatric anaesthesiology service within a university hospital in France. After several weeks of open observations, we chose to deploy an a posteriori methodology: scenarios of real incidents were collected after their occurrence. Indeed, observations conducted have shown that (thankfully) few incidents occur in daily practice. And although resilience is an essential quality for any type of disturbance, it is recognised that ‘these determining characteristics are often easier to note in the case of events of an unusual scale or severity’ (Hollnagel and Sundström, 2006). Indeed, the analysis of these incidents shows how the system behaves at the performance boundaries, that is, simultaneously how it adapts and adjusts to cope with disturbances and what are the limits of this adaptation (Woods, 2006a). The method chosen to collect a posteriori incidents was based on the critical incidents technique (Flanagan, 1954) and its main extension: the critical decision method (Klein and Armstrong, 2005; Stanton et al., 2005). Both techniques aim to raise ‘salient episodes’ in the practitioners’ memory: during interviews, anaesthesiologists were asked to recall and describe incidents they had experienced or to which they participated. As defined by Flanagan an incident is critical if ‘it contributes positively or negatively to the overall goal of the activity’ (Flanagan, 1954, p. 272). It is therefore theoretically possible to collect events that had a particularly beneficial impact on the success of the activity. But in practice it turns out that one obtains mostly negative events (Bisseret et al., 1999). Thus, to understand the system performance in general – both failures and successes (cf., Prologue) – our collection of scenarios focused exclusively on cases of near accidents where adaptations were successful. For many authors, it is preferable to collect recent events to get stories less distorted and more detailed (Bisseret et al., 1999; Ombredane and Faverge, 1955). But studies on episodic knowledge show that the age of the recalled events is totally unrelated to the vividness of memory. The vividness seems to be mainly connected with the emotional content of the memory (Bærentsen, 1996). Thus, in the method we deployed, no restriction was made vis-à-vis the age of the remembered episodes: we considered, as Flanagan suggests, that ‘the incidents themselves contain evidence of the accuracy of the account. If complete and precise details are given, we can consider that the information is accurate’ (1954, p. 275).
Six trained anaesthesiologists were interviewed (four of whom had many years of experience). They were asked to recall near-accident situations, in which they were close to a severe problem for the patient, but where they managed to cope and get back to a stable condition. Each interview lasted for about one hour. The instructions given to participants for verbalisations were fully prepared, because it is a crucial point for the verbalisation processes: ‘a small change in the instruction may affect the nature of the collected incidents’ (Flanagan, 1954, p. 277). The interviews were then semi structured: the interviewees spoke freely but were brought to address predefined themes. According to the critical decisions method, ‘probes’ previously selected, were used to obtain more information on cognitive processes and key decisions (Stanton et al., 2005). At the end of the interview, two open questions were asked in order to conclude.
In your opinion, which factors enable a team of anaesthesiologists to cope with emergencies?
Are some events easier to recover than others?
These questions aimed to make the respondents see the connections between the episodes mentioned during the interview and to compare them. According to the critical incident technique, data processing was mainly qualitative and subjective: it consisted in building a classification of events collected. This is the ‘classification criteria and the values they take that made the outcome of the study’ (Bisseret et al., 1999, p. 127). Interviews were thus transcribed and a content analysis was performed.
Unforeseen Situations: Potential Variability and Unthought-of Variability
Twenty-two situations of near accidents, dating from ‘a few days’ ago’ to ‘20 years ago’, were recalled by anaesthesiologists during the interviews. They allow us, as a first step, to draw up some characteristics of near accidents marking the memory of anaesthesiologists. The first characteristic of these scenarios concerns the severity of the situation. All of the situations reported are situations where the patient’s life was at stake, for which the anaesthesiologists said they narrowly avoided the death of the patient. The second characteristic refers to the temporal dimension of scenarios remembered: most situations are acute situations where time passes very quickly, where monitored parameters are changing ‘brutally’ and where anaesthesiologists must act in urgency. A third feature concerns the emotional content of narrated episodes: in half the cases, interviewed practitioners spontaneously evoked memories of ‘fear’, ‘stress’, ‘concern’ or ‘anguish’. One last point relates to the unexpected nature of the situation: all recollected situations were characterised by practitioners as unexpected events. But a more detailed analysis of the scenarios shows that the concept of ‘unforeseen’ is vast and includes many different situations. It is also mentioned by some practitioners that ‘there are levels of unpredictability’ that some episodes are ‘more or less predictable than others’. Indeed, unexpectedness can arise in different ways. An unforeseen situation may be a situation that was already envisaged as possible by the anaesthesiologist before the intervention. In this case, the unexpected is not directly related to the event but to the time of the occurrence of this event, that could not be determined with certainty by the practitioner before surgery. These situations are potential situations. At the opposite, a situation may be unexpected in its very nature: the event itself has not been foreseen by the anaesthesiologists. The situation is not surprising because of its unexpected occurrence but because of its very nature, which has not been thought of. These situations were unthought-of situations when they occurred. The distinction between these two types of unforeseen situations defines two areas.
• The area of potential variability, which corresponds to the situations that the anaesthesiologist considers a priori as likely to occur during surgery.
• The area of unthought-of variability, which corresponds to the situations which are not envisaged by the anaesthesiologist before surgery.
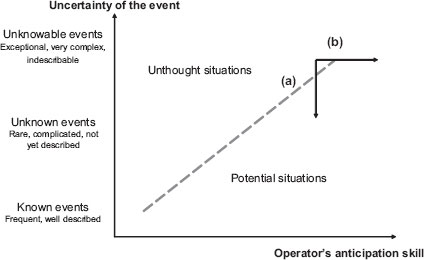
Unlike the ‘adaptation areas’ and the ‘states of resilience’ presented above, this classification is subjective since it relies on a categorisation of situations as they were experienced by the subjects: it takes into account the operators’ point of view on the events, in a given context, when the event occurred. This distinction is based on an ergonomic activity analysis, that is, on ‘an analysis of the strategies (regulation, anticipation) developed by operators to manage the gap between the prescribed task and the actual work’ (Guérin et al., 1997). The goal is not to characterise the rarity or the ‘objective complexity’ of the event as seen by a subject outside the action (Leplat, 1988) but to describe ‘the astonishment of the perceiver’ (Weick, 1993, p. 633) and therefore, this classification takes into account the way in which the situation was envisaged before surgery. Figure 3.1 places these two areas in the model of ‘the resonance in complex systems’ proposed by Hollnagel (2004).
Figure 3.1 Schematic representation of the categorisation of collected episodes
Note: each episode is classified either as an unthought-of situation, or as a potential situation, according to the operator’s perspective in the incident’s circumstances
This distinction between potential and unthought-of situations was used to categorise the 22 recalled incidents, as illustrated by the two episodes summarised below. Table 3.1 shows the distribution of the 22 episodes, according to this classification and according to the physician who related them.
Potential situation: A patient who never underwent general anaesthesia must be operated on urgently. The intubation is very difficult and the anaesthesiologist cannot put in place the breathing tube. To face, he ‘follows the protocol to the letter: several attempts at intubation, chuck, then fast track’. This event is described as ‘unexpected’ because the anaesthesiologist could not know with certainty in advance that this intubation would be a difficult one: the assessment of risk criteria usually made during the pre-anaesthetic visit, has not been made. But this possibility has been considered: ‘it is a situation that every anaesthesiologist feared more than anything in urgency’. ‘I had considered the worst’.
Unthought-of situation: At the end of an intervention, when being transferred in the recovery room, the child becomes black, cyanotic and bradycard. The anaesthesiologist begins the resuscitation and calls for help. Two colleagues arrive and take turns to perform cardiac massage. In parallel, the three anaesthesiologists think together in order to understand the event: checking equipment, clinical diagnostics, radiological examination. After 45 min, the diagnosis is made (pneumopericardium). One of the anaesthesiologists performs the technical gesture that will bring the child back to a stable state. The situation is described as ‘exceptional’. The physician in charge of the patient did ‘not imagine at all that it could happen’. ‘I thought that things would proceed as usual’.
Table 3.1 Distribution of the 22 recalled cases of near misses

Resilience as the Ability to Define an Envelope of Potential Variability
Nine situations have been categorised as critical situations where the unexpected refers to the time of the occurrence of the event. These potential situations are described as relatively frequent ones: the anaesthesiologists ‘could watch for it at each intervention’. (In the following, excerpts from the transcript are in italics.) In this case, similar stories are told several times by different anaesthesiologists. These situations are always related to the clinical evolutions of patients and do not involve physical or organisational surprise: the events are known events in the field of anaesthesia, learned during training and well described in the literature of the speciality. To handle these situations, care protocols are directly applied. The necessary resources, such as equipment or drugs are available and have been prepared beforehand. In particular, practitioners never called for additional help during the surgical operation: when, in some cases (2/9), the cooperation of two anaesthesiologists was necessary, they worked in pair from the beginning of the intervention. At the extreme, in one case the anticipated risks are such that the two anaesthesiologists decided in agreement with the surgeon, not to perform the operation.
In these nine situations, the adaptability of the system depends on the operators’ ability to define an envelope of potential variability before each operation, that is, a set of situations that may occur; in case of which the necessary resources to face are prepared. This envelop is based on the ‘objective level of uncertainty’ of each event, according to the originality of the event in the field of anaesthesia. For a given operator, the events are more or less uncertain because, according to their degree of novelty, they are more or less known and listed in the field: the relatively common events, such as difficult intubations or spasms, are described in the literature (experts’ recommendations, consensus conferences, rules of ‘good practices’ in services, etc.) making them more predictable, while very rare events, involving, for example, a technical failure and the development of a new clinical pathology are unknown (even unknowable) and very uncertain. For most clinical hazards related, anaesthesiologists mentioned these ‘indicators’, used to estimate a priori the occurrence probability of the event. Some of them are related to diseases: they are codified in the algorithms of care and systematically evaluated before each intervention. But these indexes are not ‘always completely reliable’ and their evaluation is closely ‘tied to experience’. Among the scenarios collected, five were unthought-of situations when they occurred although these events are identified and known in the field of anaesthesia.
Moreover, other indicators, related to the overall situation of the surgery, are mentioned. For example, some indicators relate to the type of surgery scheduled or to the surgeon who will perform it. Indicators may also include features related to the period of intervention. Finally, in some cases, it is difficult for practitioners to explain the elements that allowed them to anticipate the occurrence of the scenario: they ‘felt’ the event or they ‘saw it coming’ ‘without knowing exactly why’ as in the quote below.
So I’m going to intubate. And while I have no criteria of difficult intubation and there, it will seem to be paranormal, but ‘I have a bad feeling’. I said to myself: ‘It stinks. I’ll put the child flat to intubation, but I do not know why, it will go wrong’. It’s a feeling we have from time to time in medicine. Certainly there are a lot of experiences behind that are probably unconscious.
Therefore, a same event can be a potential or an unthought-of situation according to the operator who is facing it. It depends on the ‘capacity [of each one] to project [himself] into future through the current, local, short-term [conditions]’ (cf., Chapter 16; Nyssen, 2008). This anticipatory capacity is linked to the experience in the trade, and in particular to the salient situations experienced during practice, as illustrated by this quotation.
For sure, now, if I have to deal with a lumpectomy I think I will order blood immediately, having been in a situation that was a factor of anxiety, very high anxiety, I will try to avoid generating this anxiety in another situation that seems similar. I will say: ‘Last time, if only I had blood’. So I will order blood.
Figure 3.2, adapted from the Leplat’s graphic on complexity of tasks in work situations (1988), presents the relation between these two variables: ‘uncertainty of the event in the field of anaesthesia’ and ‘operators’ skill to anticipate the future’. It shows two regions corresponding to the two categories of collected episodes.
The region of potential situations is where the operator’s expectation outweighs the uncertainty of the event. This area corresponds to either well known and well described events for which ‘all anaesthesiologists are preparing all the time’, or to less known and more rare events managed by experienced operators whose ability to imagine the future is more efficient.
Figure 3.2 Predictability of a given situation for a given individual
The region of unthought-of situations where the uncertainty of the event overrides the physician’s ability to anticipate the situation. This region corresponds to inexperienced operators or to experienced operators faced with unknown situations.
The analysis of these potential situations leads to a first approach to resilience: to increase the system’s ability to adjust to variability, we must avoid the occurrence of unthought-of situations, which means making situations more predictable so that resources can be anticipated beforehand. The graph shows two possible improvement ways.
The first (a) is to increase knowledge about risk situations. To do this, different possibilities are open in the medical field (basic research on diseases including identification of warning signs) and in the field of reliability (modelling types of potential problems and identifying warning signs, through the analysis of past incidents for example (cf., Chapters 7, 15 and 17).
The second (b) is to develop the operator’s ability to project themselves into future in real conditions (cf., Chapter 16). This is the path of vocational training and especially of training based on the analysis of practices and on reflective activities (Falzon, 2005; Mollo and Falzon, 2004) that may aim for example, at ‘clarifying the foreboding’ or highlighting ‘embedded’ expert’s knowledge.
Resilience as the Ability to Diagnose that the System Leaves the Envelope of Potential Variability
Thirteen of the 22 cases collected are situations that were not envisaged by the anaesthesia team in charge of the patient before their occurrence. In the recalled stories, these situations are described as exceptional. Indeed, the 13 situations related are unique: there is no similarity between the different cases scenarios. But, as mentioned previously, in five cases, the unthought-of situation, which surprised the practitioner during the surgical intervention, concerned solely the patient’s clinical course. And, ultimately, it proved to be a known pathology, described in the literature and for which procedures are defined (e.g., pneumopericardium). The other cases (eight) are situations that involve an organisational or technical unexpected event, like breakdown of equipment or problems of cooperation with the surgical team, as illustrated by the case summarised below.
The child who must undergo surgery presents a latex allergy. The anaesthesiologist informed of this fact, put all the measures in place to prevent the occurrence of this allergy: the operation is scheduled early in the planning, all materials containing latex are removed from the operating room, the whole team is informed. After the patient asleep, the anaesthesiologist leaves the room to care for another surgical operation and lets the anaesthesiologist resident monitoring and controlling the surgery of the allergic child. He is recalled after a few minutes because the child has an anaphylactic shock (a severe allergic reaction). The possibility of an allergic reaction to latex has been anticipated by the anaesthesiologist but it is unthinkable for him that there is latex in contact with the child, since he has made every effort to remove all the latex from the operating room. The fact that the resident has picked up a protection sensor in latex outside the room is, at this moment, an unimaginable event. To cope with the situation, the anaesthesiologist calls a colleague for help, who quickly detects the latex in the child’s nose.
Although the situation has not been considered before its occurrence, it was sometime (2 cases out of 13) immediately understood and managed through the strict application of an existing protocol. But in the most cases of unthought-of situations, the strict application of existing protocols cannot directly deal with the event (11 stories out of 13). In these cases, anaesthesiologists had not envisaged such a situation and were in difficulty.
Identifying and Understanding the Situation
The diagnosis is not immediate, the sense of what is happening is lost (Weick, 1993), and since the problem is not identified, it is impossible to implement a protocol and to bring the situation with certainty in stable condition. The anaesthesiologist is here confronted with the cognitive trade-off for managing dynamic situations (Amalberti, 1996): he must choose between understanding – that is, maintaining an unstable survival state of the patient to pursue his reasoning and establish a correct diagnosis before acting – and agreeing not to understand that is, choosing one of the possible protocols, according to the hypotheses of diagnostic.
Implement Ways to Cope
The situation is understood but protocols cannot be applied because provided technical gestures do not work or surgical teams do not meet the demands of the anaesthesiologist. The anaesthesiologists may then either continue to apply an inefficient protocol provided by the organisation, or he may conduct actions ‘beyond protocols’.
In both cases, physicians must take decision(s) based on the assessment of the risk/benefits ratio of the different options, generally under very high time constraints. Based on these decisions, additional resources are mobilised according to the specificity of each situation: medical examinations (such as radiology), blood order for transfusion, use of emergency drugs etc. In particular, we note that in nine of these 13 unthought-of situations, the anaesthesiologists called on colleagues for help. Thus, calling for help appears as a transversal strategy for the different unthought-of scenarios collected. Earlier results (Cuvelier and Falzon, 2008) have shown that this call for help is not simply related to the identification of a need (estimation by the practitioners that the resources provided inside the envelope of potential variability are insufficient) but is rather a trade-off decision between multiple criteria: the availability of colleagues, the time of the day, the function of the call etc. These decisions to mobilise additional resources (and in particular to call a colleague) are the observable signs of the shift of the system from a ‘thought-of’ state considered a priori as potential, to an ‘unthought-of’ state. In this sense, they have been described as ‘pivotal decisions.’ Resilience in these unthought-of situations lies thus in the operator’s ability, not only to detect, but also to decide that the system leaves the envelope of potential variability.
Enhancing Resilience: Paths for Progress
This study highlights the role of two crucial decisions in the management of uncertainty by anaesthesiologists. The identification of these two decisions provides opportunities for research and actions to improve resilience in the practice of anaesthesia.
The first decision is the preoperative definition of an envelope of potential variability of the surgical intervention. Results show that the construction of this envelope does not only depend on the situation’s level of uncertainty (frequency of occurrence, objective prediction criteria, etc.), but also on the ability to project oneself into the future, an ability which is closely tied to experience. In this perspective, an investigation of the way in which anaesthesiologists construct the envelope of potential variability, taking into account the role the experience in this construction, would be helpful. One possible avenue for improving the resilience could be that of training through reflective practice. Moreover, the definition of the ‘envelope of potential variability’ may also be questioned at various organisational levels in the system and between different trades: is, for example, the envelope of potential variability defined by the anaesthesiologist, consistent with the one defined by the surgeon or with the one defined by the management staff?
The second decision concerns the occurrence, during the operation, of an unthought-of situation which trespasses the envelope initially defined. In such a situation, anaesthesiologists may or may not understand the problem. But in all these cases, they must decide if the problem can be managed with the resources provided in the envelope, or if the mobilisation of additional resources, including the call of colleagues, is necessary. Another area for further study is to investigate the mechanisms of this decision on the spot, using simulators and in depth recall interviews. It consists not only in identifying the factors involved in this decision (severity of the situation, changing dynamics of the process, availability of resources etc.) but also in understanding how the practitioner evaluates their own capacity to manage the event. Once again, the role of experience can be questioned, wondering, for example, if the decision taken by a novice to call a colleague in an unthought-of situation (that is unpredictable for this person in this context, so not necessarily very complicated) is based on the same mechanisms as the decision to call for help made by an expert in an unknown situation.
This study is supported by a grant from the ‘Haute Autorité de Santé’ (France). We thank the anaesthesiologists who agreed to participate in this study. We also wish to thank Professor Leplat for his availability and his interest in our work.