The effects of benzodiazepines on behavioural aggression
INTRODUCTION
Benzodiazepines have been in clinical use since the early 1960s. Initially they were claimed to have anti-aggressive as well as anxiolytic properties, although the animal literature has been equivocal (Rodgers & Waters, 1985), differing according to species and test. Reports of rage attacks in humans occurred early on (e.g. Boyle & Tobin, 1961) and were labelled paradoxical reactions as they tended to occur in isolated instances and usually at high doses (Bond & Lader, 1979). Reports have continued with the newer benzodiazepines (Rosenbaum et al., 1984). Laboratory studies have suggested that chlordiazepoxide and diazepam but not oxazepam increase hostility or aggressive responding (Gardos et al., 1968; Salzman et al., 1974, 1975; Wilkinson, 1985).
It is thus possible that benzodiazepines differ in their propensity to release aggressive behaviour. Increasing awareness of problems with the benzodiazepines, e.g. dependence and amnesic episodes, has led to attempts to differentiate among them. Duration of action has been used as one attribute, short-acting compounds being assumed not to accumulate, although offset of effect may be disconcertingly abrupt (e.g. rebound insomnia). However, other parameters have also been suggested as relevant, for example, potency and ceiling efficacy. The former refers to the dosage required for a criterion effect, the latter to the maximum effect irrespective of dosage.
One way to investigate these putative differential effects is to compare two compounds of similar pharmacokinetic properties at comparable doses (to obviate potency differences) to see whether the profile of activity differs. If it does, and potency differences really have been taken out of the equation, then the results probably reflect genuine efficacy differences. This in turn has implications for hypotheses concerning the mode of action of the drugs at the receptor level and also for the development of newer benzodiazepine-like drugs with improved risk/benefit ratios.
Two intermediate-acting benzodiazepines that have both been used extensively to control daytime anxiety are lorazepam and oxazepam (Greenblatt, Shader, Divoll, & Harmatz, 1981). They differ in structure by only one chlorine atom but they have different clinical potencies, lorazepam being 15 times more potent than oxazepam. Also, ceiling efficacies seem different, lorazepam being much more likely to impair memory functions at an equivalent clinical dose (Curran, Schiwy, & Lader, 1987). As oxazepam has not been implicated in either rage attacks or hostility engendered in a laboratory paradigm, it seemed an ideal comparison for the more potent lorazepam in our competitive reaction time task. The two drugs were used in doses that were considered, according to the official Data Sheets, to be equipotent in the clinical control of anxiety.
Methods
Subjects
Subjects were recruited via advertisements posted on the institutional notice-board. They were paid for participating. Forty-five normal healthy volunteers took part in the study, 20 females and 25 males. Their age range was 19–46 years with a mean age of 26 years. They were divided into five groups, each with 4 females and 5 males.
Drugs and procedure
The study was approved by the appropriate Ethical Committee and written informed consent was obtained from all subjects. A double-blind independent five-group design was used to compare the treatments: oxazepam 15 and 30mg, lorazepam 1 and 2mg, and placebo. Subjects were instructed not to take any alcohol or other CNS drugs for 24 hours before testing and not to take substances containing caffeine on the test day. The ratings were completed before and 4 hours after drug administration and after the competitive reaction time task (4.5 hours post-drug). The competitive reaction time task was run starting 4 hours post-drug.
Measures
Competitive reaction time task
This was run as detailed in Chapter 3. Physiological measures were also recorded during the task, again as described in Chapter 3.
Subjective rating scales
The Mood Rating Scale, Anger Rating Scale and Spielberger State-Trait Anxiety Inventory were administered as set out in Chapter 3.
Analysis of data
Multivariate analysis (between groups, time, sex, and the interactions thereof) was used to analyse data both for the ratings, which were measured three times, and for the variables measured on the four blocks of trials of the CRT task. Patterns of trends over time were examined and contrast analysis was used to evaluate differences in treatments with the following planned pair-wise comparisons: placebo versus active drugs; oxazepam versus lorazepam; high doses versus low doses.
Results
Competitive reaction time task
Level set – Trial 1 (nonprovocation). The drug groups did not differ on Trial 1. Males in all groups set higher levels than females (F1,33 = 4.48; P<0.05).
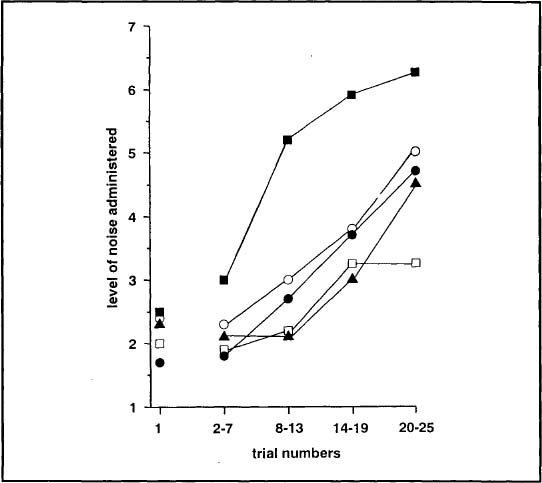
Trial blocks 1–4 (increasing provocation). Males continued to set higher noise levels than females overall (F1,33 = 4.58; P < 0.04) and subjects on active treatment set higher levels than those on placebo (F4,33 = 3.52; P < 0.02) (see Fig. 6.1). All groups set higher levels with increasing provocation (F3,31 = 31.24; P < 0.001 but the groups differed with respect to the size of this increase (F12,82 = 2.15; P < 0.03) (see Fig. 6.1). Levels were significantly higher in the high dose lorazepam than the high dose oxazepam group (F1,33 = 5.08; P < 0.04). An interaction occurred between high and low doses and time (F3,31 = 3.35; P < 0.04): The high dose of lorazepam showed most increase. There were no drug effects on setting time or reaction time.
FIG. 6.1. Mean levels of noise administered by subjects after lorazepam 1mg (![]() ), 2mg (
), 2mg (![]() ) oxazepam 15mg (
) oxazepam 15mg (![]() ), 30mg (
), 30mg (![]() ), and placebo (
), and placebo (![]() ) during each block of trials of the CRT.
) during each block of trials of the CRT.
Physiological measures
Skin conductance level and fluctuation
Trial 1. There were no significant differences between groups on the basal level of skin conductance, the change within trial, or the number of fluctuations on trial one. Fluctuations increased from pre-trial to during the trial (Fl,37 = 38.43; P < 0.001).
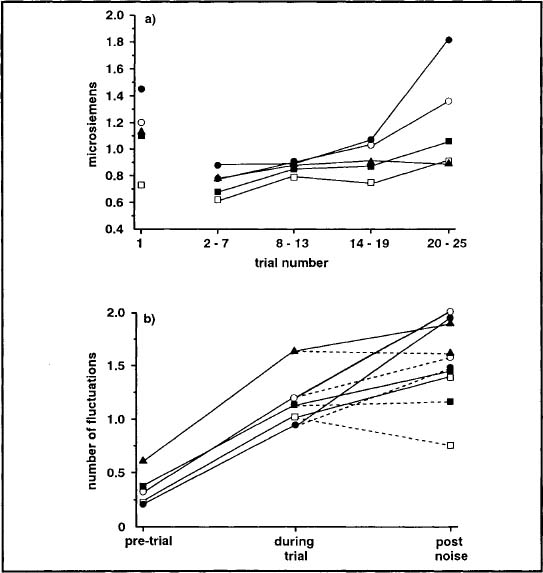
Trial blocks 1–4. All subjects showed an increase in baseline skin conductance level through the experiment (F3,30 = 40.59; P < 0.001). There was no difference between drugs. The change in level within each trial also showed an increase through the experiment (F3,30= 6.98; P < 0.01) but the drugs × times interaction also showed a significant quadratic trend (F4,32 = 3.23; P < 0.05). The subjects on oxazepam showed more change within trial as the experiment progressed. The number of fluctuations increased through the experiment (F3,35 = 4.31; P < 0.01) and showed a highly significant difference within trial between conditions (F3,35 = 81.67; P < 0.001). Fluctuations increased from pre-trial to the rest of the trial and from during the trial to after the RT and there were more fluctuations after the noise than when no noise occurred. There was a significant interaction between condition and drug (F12,92 = 1.95; P < 0.05). Subjects on oxazepam showed a greater increase in fluctuations from during the trial to after the reaction time (see Fig. 6.2).
FIG. 6.2. Mean (a) skin conductance levels during each block of trials and (b) number of fluctuations within trial. The dashed line (- - -) represents when no noise was administered. Values shown after lorazepam 1mg (![]() ), 2mg (
), 2mg (![]() ), oxazepam 15mg (
), oxazepam 15mg (![]() ), 30mg (
), 30mg (![]() ), and placebo (
), and placebo (![]() ).
).
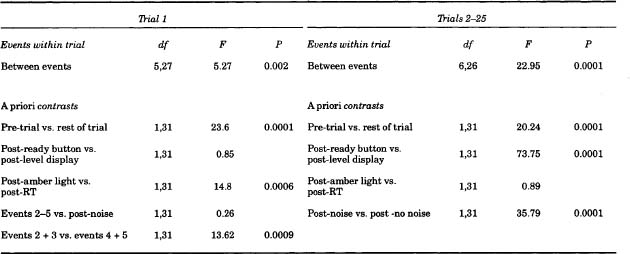
Heart period
Trial 1. The heart period showed a similar pattern of effects (see Table 6.1) as found previously (Chapter 5). It shortened from immediately before the start of the trial to subsequent points within the trial and from after the warning signal for the reaction time (RT) to after the RT itself. The drugs did not alter this pattern but there was a drug × type interaction on the change from resting level to events within trial (F4,31 = 4.57; P < 0.01). The high dose of oxazepam group showed a greater change than the other groups.
Trial blocks 1–4. The heart period again showed a distinct pattern of effects (see Table 6.1). It shortened from pre-trial to events within trial, from no noise to noise condition, and it lengthened from after the subjects had set the noise level to be delivered to their opponent to after the display of the level they themselves would receive. This pattern was not affected by the drugs. There was an overall significant difference between drugs because subjects on both doses of oxazepam had a longer heart period than those on placebo or lorazepam (F4,31 = 5.71; P < 0.01). There was also a significant effect across trial blocks (F3,29 = 4.13; P < 0.05). The heart period initially became longer but then shortened through the experiment. There was no significant interaction with the pattern within trial.
Subjective rating scales
Mood rating scale
Factor: 1 alertness. All subjects became more drowsy 4 hours after drug administration (F1,33 = 14.73; P < 0.001) and then more alert after the task (F1,33 = 74.52; P < 0.001) (see Fig. 6.3a). The subjects on active treatment became more drowsy than those on placebo (F1,33 = 3.03; P < 0.05) but there was no difference between groups post-task.
Factor 2: contentment. There were no drug effects on this factor but the females in all groups were more discontented than the males, both before and after tablet administration and the task.
Factor 3: calmness. The subjects in all groups tended to become calmer post-tablet administration (F1,33 = 4.07; P < 0.06) and more tense post-task (F1,33 = 24.66; P < 0.001) (see Fig. 6.3b). There were no drug effects.
TABLE 6.1
Multivariate analysis of variance of heart period between events within trial with a priori contrasts
FIG. 6.3. Mean scores on (a) Factor 1 (alertness) and (b) Factor 3 (calmness) of the mood rating scale.Values shown after lorazepam 1mg (![]() ), 2mg (
), 2mg (![]() ), oxazepam 15mg (
), oxazepam 15mg (![]() ), 30mg (
), 30mg (![]() ), and placebo (
), and placebo (![]() ).
).
Anger rating scale
Twelve of the 13 items of the ARS showed significant effects over time. The subjects rated themselves as more peaceful post-drug (10 items) and more angry post-task (12 items) (see Fig. 6.4). Only one item (belligerent-restrained) also showed an interaction between drugs and time (F4,33 = 3.38; P < 0.02) and a difference between high and low doses on this interaction (F1,33 = 9.16; P < 0.01). Subjects on the high doses of lorazepam and oxazepam rated themselves as significantly more belligerent after the task than before it.
FIG. 6.4. Mean scores on VAS angry-peaceful pre-drug, 4 hours post-drug and post-CRT. Values shown after lorazepam 1mg (![]() ), 2mg (
), 2mg (![]() ), oxazepam 15mg (
), oxazepam 15mg (![]() ), 30mg (
), 30mg (![]() ), and placebo (
), and placebo (![]() ).
).
Spielberger State-Trait Anxiety Inventory
There were no significant differences between groups on the STAI-Trait, administered before the experiment. The mean score was 37.7. There were no significant differences between groups on the STAI-State. Subjects in all groups became more anxious after the task (F1,33 = 8.87; P< 0.01).
DISCUSSION
Lorazepam and oxazepam are very similar in structure and pharmacology and might therefore be expected to have a similar profile of effects in the tests we used. This was so for the subjective measures: Some sedation was shown after both drugs but neither showed anxiolytic effects compared with placebo. However, the two drugs diverged with respect to their effects on the competitive reaction time task. Although initially the same, the groups became differentiated as the trials progressed. All groups increased the volume of the noise they intended to administer to their "opponent" but the high dose lorazepam group selected the highest noise levels. Nevertheless, the groups generally did not differ in their self-ratings of anger or hostility. The doses of each drug used were believed to be equipotent in clinical terms and produced comparable levels of sedation. The lower dose levels of the drugs were indistinguishable, and they only diverged at the higher dose. This raises the question as to whether even higher dose levels of oxazepam would have induced hostility comparable to that of the 2mg dose of lorazepam. However, excessive drowsiness would probably preclude testing.
Could the differential effect merely reflect potency as a factor rather than ceiling efficacy? Lorazepam is 15 times more potent than oxazepam. Potency is generally regarded as unimportant for clinical purposes (Gilman, Mayer, & Melmon, 1980) but it may have some relevance for adverse effects. More problems are generally encountered in withdrawing patients from benzodiazepines with short elimination half-lives and high potency (Martinez-Cano, Vela-Bueno, de Iceta, Pomalima, & Martinez-Gras, 1995; Tyrer, Rutherford, & Huggett, 1981). Alternatively, the difference may be related to ceiling efficacy, and lorazepam may exert a maximal effect on such behaviour at a lower equivalent dose than oxazepam. Disproportional effects of this dose of lorazepam have also been displayed on memory functions (Curran et al., 1987). Comparisons between diazepam, oxazepam, and lorazepam found only lorazepam to impair implicit memory (Curran & Gorenstein, 1993; Sellal et al., 1992).
Could differences in peak effect have accounted for this disparity? Testing was carried out 4 hours after drug administration, as from previous studies this was deemed the most appropriate time. Data from another study using 1.5 and 3 hours testing times showed oxazepam to have a later onset of action than lorazepam (Curran et al., 1987), and lorazepam has been shown to produce more subjective sedation and psychological impairment at 4 hours than at 1.5 hours after administration (File & Bond, 1979) and so the effects of the two drugs should be equivalent at 4 hours.
The competitive task produced characteristic effects on the physiological indices. The skin conductance data showed a distinctive pattern, basal levels and reactivity increasing over the task. The drugs had no effect on the resting level, but subjects on oxazepam showed more response to events within each trial as the provocation increased, and more fluctuations at the end of the trials. Thus, the increased noise set by the subjects given lorazepam was not part of a general hyperreactivity. The heart period (inter-beat interval) changes showed distinctive patterns within trial similar to those found in our other studies. There were also changes across trial blocks. The heart period lengthened as subjects became familiar with the task and then shortened again (tachycardia) as the noise increased. Oxazepam had more effect on the resting heart period than lorazepam throughout the task but it did not block change within trial. This effect may then have been due to differences in initial values between subjects.
Pro-aggressive actions have been shown for other benzodiazepines tested in the laboratory. Chlordiazepoxide, but not oxazepam, increased hostility in a group setting after a frustrating stimulus was introduced (Gardos et al., 1968; Salzman et al., 1974; Kochansky, Salzman, Shader, Harmatz, & Ogeltree, 1975, 1977). Diazepam increased hostility in a group of females (McDonald, 1967) and behavioural aggression on the competitive reaction time task utilising shocks (Gantner & Taylor, 1988; Wilkinson, 1985). The latter study attempted to relate levels of trait anxiety to aggression, but although a relationship was found on the first block of trials (low trait anxiety subjects on diazepam showing most aggression) as provocation in the form of shock level increased, all subjects on diazepam showed greater behavioural aggression than those on placebo. The present study shows lorazepam to have similar effects to diazepam and chlordiazepoxide and confirms the finding that oxazepam does not affect behavioural aggression (Salzman et al., 1975).
The lack of anxiolytic effect of the two benzodiazepines needs comment. Such effects may not occur regularly in normal subjects with low or even moderate levels of anxiety (Spielberger et al., 1970) except under extreme anxiety-provoking conditions. But even if an anxiolytic effect is induced, aggression may increase as shown by the effects of alcohol in the study presented in Chapter 5.
SUMMARY
Two doses of two very similar benzodiazepines (oxazepam 15 and 30mg, lorazepam 1 and 2mg) and placebo were compared 4 hours post-administration on a competitive reaction time task designed to measure behavioural aggression. Forty-five subjects were assigned randomly to five independent drug groups. Subjective ratings of mood, anxiety, and aggression were completed pre- and post-drug and post-task. Oxazepam and lorazepam had very similar subjective effects but oxazepam produced more physiological reactivity. The higher dose of lorazepam increased aggressive responding on the task more than any other treatment. This may be related to the different ceiling efficacies of the two benzodiazepines.