Chapter 7
Systems of Systems in the Healthcare Field 1
7.1. Introduction
The medical field is undergoing major changes. Clinical exams are more and more often instrumented through the implementation, direct or indirect, of computerized systems. The same applies for the administrative data exchanged between hospitals and social security administrations when you (the patient, us!) are hospitalized. The ophthalmologist runs a digitalized dilated fundus oculi examination, which he stores in the patient’s file, in his computer. The patient uses his health insurance card so the health professional can create a file for the reimbursement of the medical procedures by social security, and pays the pharmacist with the card of his complementary health scheme. Those are only the most visible aspects of the evolution, rooted in the information world, which the medical field is currently going through.
The medical field is characterized by the diversity of its organizations (public or private hospitals, pharmaceutical industry, technical medical systems industry, health insurance funds, etc.), its agents (health professionals, working in health facilities or private practices), these agents’ activities (medical or paramedical agents, social workers, etc.), and the technical systems supporting their activities. The diversity of organizations, agents, activities and technical systems, favors their interaction, to exchange data, design healthcare networks, record the procedures undergone by the patient through his entire life and manage the healthcare systems.
We can already see the outline of the services which the systems of systems – independent systems which, when interconnected, provide new services and enrich the value chain – could be expected to provide in the medical field.
This chapter is broken down into five parts:
– the first part defines the challenges, in terms of capability, around which systems of systems are designed in the medical field;
– the second part characterizes the medical field’s systems in terms of services provided;
– the third part studies the coordination of the agents’ activities within the healthcare networks;
– the fourth part looks at the development of the information technologies and their interoperability, at the heart of the issue of healthcare networks;
– finally, the fifth part studies the difficulties met in the field.
This chapter was elaborated from information sources and interviews (in alphabetical order): Karima Bourquard, Yves Constantinidis, Claude Pourcel, Jean-Claude Sarron and Michel Veret.
Currently, many initiatives are led in this field and this chapter does not claim to cover them all, but rather to shed light on the issue of systems of systems in the healthcare field.
7.2. From capability challenges to the design of systems of systems
Population development (increasing number of dependent elder people), societal (refocus the healthcare system on the patient) and financial (reduce the costs of healthcare systems and optimize the use of resources) evolutions, as well as the development of healthcare networks, all require the global healthcare system to undergo major changes.
Indeed, the efforts in placing the patient back at the heart of the healthcare system, the shortage of practitioners, the search for the continuity of service and the implementation of information technologies bring about a search for increased capability in order to:
– improve patient care quality, whether on a medical level (quality of care) or a social level, as well as improve quality of life (for example by helping the patient stay at home whenever possible);
– improve the coordination of the various medical and paramedical agents, working in hospitals or private practices, who contribute to the medical care services, through the optimization of processes and channels;
– successfully manage, optimize and use hospital resources (to fully profit from an expensive scheme);
– garner expertise wherever it may lie, without its localization penalizing patient care quality;
– successfully handle the ageing of the medical profession;
– improve the care’s cost/performance ratio.
This heightened capability can be achieved through several means, including the development of healthcare networks outside of the hospital, and the integration of the various healthcare activities within one continuous service, focused on the patient. This can be achieved through the implementation of information technologies.
Our discussion is in the context of systems of systems, such as defined by Maier (Chapters 1, 2 and 4). Indeed, the agents of the healthcare networks, the health facilities, the general practitioners, etc., are independent on an operational level, each with their own activity not dependent on the others’. They are also independent on a managerial level, since physicians can work in private practices, and health facilities can either be public or private organizations. The medical and paramedical agents are scattered within a more or less important geographical and demographical basin. Network-centric operation enables the provision of services which no individual agent could deliver. These networks are organized thematically: pediatric networks, oncology networks, etc. Lastly, in order to provide their services to the patients, the medical and paramedical agents must coordinate their activities and exchange medical and paramedical information about the patients.
This system of systems features a major and structuring characteristic. Its purpose is to provide services to the patients, who are an integral part of the healthcare process.
Figure 7.1 places the patient at the heart of the healthcare process, which features a set of health professionals, working either in hospitals or private practices. A network can feature several hospitals and several private practitioners within one population pool.
Figure 7.1. Patient at the heart of the healthcare system (source [GIU 01])

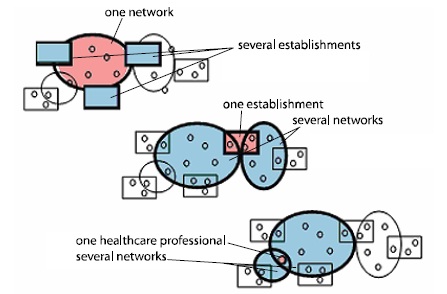
If a network can feature several health facilities, a hospital can contribute to several networks. Likewise, private practitioners can contribute to several networks, as demonstrated in Figure 7.2.
Figure 7.2. Hospitals and health professionals within and at the intersections of the healthcare networks (source [GIU 01 ])
We delimit three sets of themes to study in order to achieve those goals and improve capability:
– the service provided to the patient, the main characteristic of systems in the healthcare field;
– the coordination of the various medical and paramedical agents activities, on an organizational level, in order to provide that service;
– the development of information technologies, to support such coordination and exchange information.
To this purpose, the information systems of the various agents of the healthcare network must be interoperable.
These are the three themes we are about to discuss.
7.3. Personal service, the main characteristic of systems within the healthcare field
If we look back at the definition of the notion of system that we have given in Chapters 1 and 4, a system is characterized as being a product or service, implemented by the final user, the processes and activities needed to supply that product or service, the resources needed for its design, its production. Moreover, we differentiate the “system to do” and the “system to be done”. The former qualifies the product, as well as the related data. The latter qualifies the set of means, processes, methods, tools, which need to be implemented in order to do, to realize the system to do.
With the healthcare field, we are not in a context of industrial production, traditional of engineering approaches, but in a context of service supply, currently identified as pertaining to service science, management and engineering ([ABE 05, HID 06, SPO 06]).
The service is therefore defined as a system of interacting parts, featuring people, technologies and commercial exchanges, with the user in direct contact with and participating in the service. Service science is multidisciplinary, calling on disciplines such as anthropology, cognitive psychology, information sciences, cognitive sciences, science education, human factors, industrial engineering, organization sociology, law, mathematics, economy and social sciences.
Abe ([ABE 05], p. 11-12), differentiates four types of services:
– services centered on specialized skills and knowledge with little connection to commodity goods, such as porters, hairstylists, gardeners, teachers, accountants;
– services which provide commodity equipment, or even goods, such as performing arts, theaters, movie theaters, museums, restaurants and caterers;
– financial services;
– services which provide information not manipulated by human beings, such as the storage or supply of information by press agencies.
In that context, the healthcare services belong to the first and second category: they include, on the one hand, services centered on the physician, the paramedical specialist, and on the other hand the services which call on a convalescent home, medical laboratory or emergency call center.
The main characteristics of a service are ([SPO 06]):
– its intangible character, which means the service provided is most often immaterial, not physical;
– simultaneousness, insofar as it is simultaneously created and used;
– its perishable character, since the service is used as soon as it is created and is therefore not preserved;
– the customer, the service’s user, actively contributes both to the creation and the use of the service;
– the difficulty to determine the quality of the service: indeed, the service’s quality is closely dependent on the interaction between service provider and service user;
– heterogenousness: the same service can have different results, depending on the provider and the state of the service’s user.
What are the impacts of this “service” dimension in the healthcare field?
The service’s user, that is to say the end user as defined by engineering, is also the “product”, which we have previously qualified by “system to do”. Indeed, the purpose of the medical procedures is to modify the state of the patient (the “product”), to “fix” him. But this “system to be done” is radically different from the products, such as they are designed in the industrial field. There is no engineering, no design of a human “product”. The human “system” is intrinsically and radically different from the object system of systems engineering. There is therefore no expression of need, specification, design, development, integration, inspection, validation, in relation to the documents concerning the specification, design, operation and disposal process.
Moreover, the patient is an autonomous subject. He actively participates in the medical service, taking or discarding the medication prescribed to him, abiding by the prescribed diets or going on with dangerous behaviors, etc. Indeed, the medical agent is not alone in providing the service which will modify the patient’s health status. The patient is co-responsible and a co-producer of this service. This service is constructed within an intersubjective relationship between the medical agent and the patient, who is at the same time the end user, the product to transform and a contributor to the service. In some way an attachment between the practitioner and the patient, a relationship of trust is built. The intimately intersubjective character of this relationship has important impacts, on the service’s realization as well as its quality, and finally on the patient’s health.
In the healthcare field, the “system to be done” is made up of the set of agents within the medical field who contribute to the service’s realization. We can therefore differentiate two main types of services: on the one hand, general practitioners, and on the other, hospitalization. These agents have organizational structures, operating modes, processes and process instrumentations, all completely different from one another. This aspect helps structure the design of the system of systems, and we will study it in section 7.4.
Just like the engineer uses data related to the product, the medical agent designs, updates, exchanges, stores data about the state of the patient, of the “product”. This is the patient file. This information also includes components typical of the implemented processes and procedures. For example, the results of a medical analysis include the protocols and developers, necessary elements to the interpretation of these results, the same way oral and rectal temperatures are both treated differently. All the information included in the patient file is unique to each individual and pertain to medical secrecy; as such, their protection is a critical factor in the elaboration of technological solutions to facilitate their treatment, storage, or exchange. The communication of these medical data must therefore be secured through mechanisms that will ensure their authentication, confidentiality, integrity and non-repudiation (see Chapter 12, section 12.21. Appendix L). The use of such personal information and the development of tools to treat them must be filed with the CNIL1. Moreover, each patient’s ID must be unique. Finally, this information remains important during the entire life of the patient, and must therefore be conserved and available all through his or her life, currently more than 100 years2.
The data concerning the patient are pertinent for a set of agents who participate in the medical or paramedical acts, or even, sometimes, for social workers. But in these situations, the agents only have access to subsets of these data.
Moreover, if the medical data and their exchange form the backbone of patient care’s continuity, the multidimensional character of the medical act means there are many more information exchanged. Besides the individual medical data (description of the medical and surgical procedures, analysis results, etc.) and the information exchanged during teleconsultations, telesurgery or telesurveillance, all pertaining to medical secrecy, there is also a non-negligible administrative part (records of performed medical procedures, billing, fee-for-service), as well as collective information of an epidemiological nature, gathered from the individual medical data, turned anonymous and aggregated, which can lead to health hazard reports and do not pertain to medical secrecy since they are no longer referencing anyone in particular.
7.4. Coordination of the medical and paramedical agents, in hospitals and in private practices
In order to ensure the continuity of the care given to a patient, the various medical and paramedical agents must coordinate their efforts, before hospitalization, during hospitalization, in all relevant departments (intensive care, radiology, surgery, specialized departments), and after hospitalization (follow-up, home care).
As we have pointed out, these various agents have different social statuses, from highly structured organizations such as hospitals and rehabilitation centers, to private practices and general practitioners, statuses which have an impact on the agents’ activities, and on their way of managing activities. As a result, it also has an impact on the coordination capacities of these various agents. What does this coordination consist of?
The hospital is an organization, with its own structure, its roles and responsibilities, its operational services and auxiliary services, such as defined by Mintzberg (see [MIN 82] and Chapter 4, for a summary of Mintzberg’s works and a definition of the various structures studied in the present section). This is not the case with general practitioners (doctor, nurse, physiotherapist, medical laboratory, etc.) who are numerous and, most often, either have a liberal status, sometimes working within private practices, or are categorized as small office/home office (SoHo), or small and medium enterprises (SMEs).
Within a health facility, the processes, the activities, are interlinked and governed by the state of the patients. A patient’s discharge is another patient’s admission and vice versa, which calls on intensive technologies ([ROJ 03], p. 134, [THO 04], p. 17-18) and reciprocal interdependence ([ROJ 03], p. 136, [THO 04], p. 55). These are complex and dynamic processes such as described by Thompson [THO 04] and Mintzberg [MIN 82]. These characteristics determine the structure and operation of a health facility.
The hospital, according to Mintzberg’s model, is mainly a professional bureaucracy. The formation required to work there on an operational level is long (medical studies or nursing schools). The work protocols are strict. The hospital is often structured into independent departments, one for every specialty (cardiology, pediatrics, obstetrics, ORL, etc.). Most of those departments tend to function autonomously, in order to reduce contingences, and are managed by a doctor, a chief resident. The development of a cluster-based organization is making this structure less automatic. Each department is then organized following a simple structure. The contingencies are reduced through the search of total control of the patient, following the logic of a total institution such as described by Goffman ([ROJ 03], p. 135, [THO 04], p. 43). The activities of the transversal departments, such as radiology, intensive care, or the internal medical laboratory, are highly dependent on one another, but these departments also define a set of constraints for the other departments, particularly in terms of resources management and use. These departments are not often in direct contact with patients, and the aforementioned characteristics do not concern them as much.
In that way, the medical laboratory, which is highly automated, would be more akin to a mechanistic bureaucracy. The strategic summit of the hospital, on the other hand, usually is not managed by a doctor but, in the case of French public health facilities, by an administrator. It is possible to have, on that level, a divided structure. Strong social differentiations can be found within the hospital, in terms of roles, responsibilities, and practices between each agent. This differentiation also translates into privileged social networks, as much within the hospital as without, in everyday life as well as in organizational and professional culture (Chapter 4).
We have seen how the patient’s active participation in the realization of the service is characteristic of the medical field, and possesses a strongly intersubjective dimension. If this intersubjective dimension is most important in the case of general practitioners, and allows for the creation of an enduring relationship between patient and practitioner, it is reduced and framed in the case of hospitalization. Indeed, if the hospital is looking for total control of the patient, the drawback is the symbolic and ritual depersonalization of the patient, such as is described by Goffman [GOF 79]. In the total institution represented by the hospital, the patient is cutoff from the outside world, completely taken care of, sometimes down to the clothes he can wear, the visiting hours are strictly regulated, the contacts between medical personnel and the patient are formalized and formatted (the health sheet at the bottom of the patient’s bed); finally, the hospital has its own temporality, notably for dining hours. This rationalization of the patient goes against the current promotion for a higher quality of life, including in the medical field, which fights in favor of home hospitalization.
Within the hospital, the coordination needed to implement the processes is based on a set of exceptional operational decisions ([MIN 82], p. 76), ad hoc decisions which are not programmed, not planned. The regulation of activity is done on a case by case basis. This is possible insofar as the patient is on the premises and available. Works are currently led on such planning and scheduling (for further information, consult the reports of the annual French GISEH conferences, “management and engineering of hospital systems”).
This is not the case, however, with general practitioners. The activity of general practitioners, medical or paramedical, is governed by their patients’ health constraints (some health services must be performed at a precise hour) and personal constraints (availability). In such a context, the coordination of their activities must be flexible so as to adapt to each other’s activity, said activity being governed by many contingent and unplanned events, and mutual adjustment systems must be implemented, such as liaison mechanisms and integrating frameworks. On the other hand, the granularity of the concerned organizations, whether they be SoHo or private practices, does not allow for the implementation of other solutions of mutual adjustment such as, for example, matrix organization.
The main components of this coordination can be formulated in terms of service request (request for medical analysis, prescription of lung x-rays, request for hospitalization, prescription of ten orthoptic sessions, etc.), replies to these requests (medical analysis results, etc.), and may include temporal or periodical constraints, as well as constraints on the way to provide the required services. Lastly, these coordinating components require the communication of medical data between the agents (medical analysis results, x-ray photos of the patient’s lungs, etc.). This medical data can be stored on an analogical medium (fax of an electrocardiogram or the results of a biological analysis) or a digital medium (barcode bracelet, digital plate, RFID3 chip for the patient file, electronic message with an attached JPEG file of an x-ray photograph, etc.).
On top of these formal aspects, the informal dimension of interpersonal relationships is necessary for coordination of the medical and paramedical agents’ activities. For example, a general practitioner can also work within the internal medical department of the hospital present in his area. His knowledge on how the hospital functions, as well as the good relationships he maintains with the doctors and the administrative staff, allow him to more easily orient patients in need of hospitalization. This accelerates and improves the coverage of patients within the hospital.
7.5. The development of information technologies and their interoperability, heart of the healthcare networks issue
We are now about to study the implementation of information technologies in the healthcare field and will then look at three major standards used to achieve interoperability of the information systems, and an example of their implementation.
7.5.1. Information technologies in the healthcare field
Information technologies help design and instrument the processes and activities which contribute to the production of care. But the situation of the medical field impacts on their definition, their development and their instrumentation.
While industrial processes can be clearly and strictly defined, organized and planned, within a logic of modeling work processes for automation (Chapter 12, section 12.8 Appendix A), such is not the case for most processes contributing to the healthcare system, insofar as the patient is directly concerned.
If hospitals implement information technologies ([GMS 07a, GMS 07b, GMS 07c]) in a structured manner, the situation is different for the medical and paramedical general practitioners, whose activities are poorly computerized. The website for the ENOSIS project states that in 2003 “less than 30% of general practitioners use a computerized medical file on a daily basis” [ENO 08].
In his 2006 report on the state of information systems in health facilities [GMS 07c], the GMSIH (Groupement pour la Modernisation du Système d’Information Hospitalier – Hospital Information Systems Modernization Group) defines the information perimeter, through the implemented process and the object of that process:
– the patient data system:
- patient’s administrative management,
- shared patient file,
- medication’s circuit,
- management of examination requests,
- management of examination results,
- management of the medico-technical units,
- emergency management;
– the economical, financial and logistical information system:
- financial system,
- the other functions (patient transportation, catering, sterilization, computer-aided maintenance management);
– the human resources management information system;
– the quality and risk management information system;
– the piloting information system;
– communication tools;
– secured exchanges with the outside world.
The evaluation report results, feedback and advice on the theme of transversal nature and master plan of the information system [GMS 07b] lays out results which we might synthesize with the following elements:
– there often are inconsistencies between the master plan, on the strategic level, and the implementation, on the tactical level, with poor involvement from the users on the operational level. On the other hand, the successful projects are characterized by a continuity between the strategic (implication of the management, of the CME4) and the tactical level, and by the users’ involvement;
– the project is rarely based on an analysis of what already exists, even though such an analysis is necessary for the integration between the current situation and what will be achieved within the project;
– oftentimes, there is no mapping based on the workflows, no architecture framework featuring the operational views;
– even if the standards of interoperability are mentioned in the master plan, sometimes in the specifications, the implementation of those standards, including the IHE integration profiles (which we will study shortly), is not explicitly required. This poses an important problem for the patient file which is, by nature, transversal.
The lack of users’ involvement has important negative impacts on quality and safety, such as violations and migrations ([HAR 2002], [AMA 09]), risks on patient safety, and considerable extra healthcare costs ([LER 09], [PEL 09a], [PEL 09b]).
We have seen the importance of interoperability in the healthcare field, a necessary condition for the information flows to correctly circulate between the sector’s various organizations. How is this interoperability managed?
7.5.2. Interoperability in the healthcare field
Since the information systems are heterogenous, interoperability lies in their ability to exchange services or data. These services or data are subject to standards, which we are about to study.
7.5.2.1. The IHE initiative
The IHE, for Integrating the Healthcare Enterprise, is an international organization, structured into networks, which allows the users and designers of information technologies in the healthcare field to reach a higher level of system interoperability through the precise definition of the activities within this field, the communication specifications based on the norms and standards between systems, and the testing of systems to determine their conformity level in relation to those specifications.
The IHE currently covers the following domains:
– cardiology;
– eyecare;
– IT infrastructure;
– laboratory;
– pathology;
– patient care coordination;
– patient care devices;
– quality;
– radiation oncology;
– radiology.
Integration profiles are developed for most of these domains. They are documents describing the solutions to specific integration problems, documenting the roles of the agents involved, and defining the details of the systems’ implementation. They ensure that everyone is talking about the same thing, without needing to breach the many technical details which in fact contribute to the interoperability.
For example, in the field of IT infrastructure, specifications or technical frameworks deal with digital signature, the exchange of clinical documents between healthcare organizations, the administrative management of patients and the directory of the personnel.
The technical frameworks define with precision the technical details of the integration profiles.
The Connectathon is a major characteristic of the IHE. This is a conference dedicated to testing the conformity of the technical solutions, in order to evaluate their level of interoperability. These conformity tests are based on real life medical scenarios and use the IHE integration profiles. This event is organized on a worldwide scale and is held, in turn, in various towns in Europe, North America or Asia: such as Chicago in February 2009, Vienna in April 2009 and Tokyo in February 2008. The Connectathon largely contributes to the credit and the broad distribution of IHE among the healthcare field’s industrialists. The organization of such an event is favored by the strong involvement of institutions, such as the INRIA in France, which provide personnel for the event. Finally, the evaluation platforms, based on web services, are easy to implement. In that context, the industrialists follow that approach and regularly perform interoperability evaluations, in-between Connectathon sessions.
To ensure the spreading of good practices and the partners’ adhesion, the IHE uses a set of resources in the form of a dedicated site (http://www.ihe.net/), and a wiki (http://wiki.ihe.net/). The wiki features many pages and many documents, technical frameworks and integration profiles.
7.5.2.2. The HL7 standard
The HL7 standard (Health Level Seven) is an exchange language located on the 7th level of the OSI (application level), hence its name, designed within HL7 Inc., taken in by the ANSI (American National Standards Institute) and used in many countries. The conceptual data model HL7 v3 is now an international ISO (International Organization for Standardization) standard, filed under ISO/HL7 21731:2006, under the title “Health informatics – HL7 version 3 – Reference information model – Release 1”.
The standard is designed by a set of technical committees (digital health-related record) and groups with specific interests, work-related (anatomical-pathology, pediatrics, cardiology, etc.) as well as technical (service-oriented architecture, etc.).
Version 2.5 features the following chapters and appendix:
– introduction to the HL7 standard;
– control: definition of the messages and the exchange protocols;
– patient management: admission, discharge, transfer, demographic elements;
– service order entry: clinical orders, orders of observation, medication, blood, imagery, dietetic food, suppliers;
– queries: the rules for the formulation of queries, and the answers to those queries;
– financial management: patient-related accounting;
– observation reporting: observation report messages;
– master files for health applications;
– management of the medical records and medical data;
– scheduling;
– referrals;
– patient care: problem-oriented records;
– clinical laboratory automation;
– application management;
– personnel management;
– data definition tables (appendix);
– low-level protocols (appendix);
– description of BNF (Backus–Naur form) messages (appendix);
– terms glossary (appendix);
– administrative aspects, such as payments, complaints and compensation requests (appendix).
Version 3 defines a set of formatted messages and includes a reference information model, a model of healthcare data, under the formats XMI, Rose, Visio, and a reference architecture of a medical file, CDA (Clinical Document Architecture) based on the XML computer language (Chapter 12).
The CDA is derived from the RIM. It allows the organization of documents with headings, highly structured so as to facilitate their indexing and sorting (document type, authentication level, confidentiality level, origin), and a body, a set of sections featuring text, images, sound, as well as multimedia content. Among other things, it treats the semantic representation of clinical events, of the patient’s vital signs (temperature, pulse, saturation rate, etc.). The sections can be, for example, medication, patient allergies, and family history.
7.5.2.3. The EHR standard
A set of alternative standards are elaborated by the CEN (Comité européen de normalisation, European Standardization Committee), under the reference CEN prEN 13606, under the name “Electronic Healthcare Record Communication” (EHRcom). This standard is present on the ISO level under the reference ISO 13606-1:2008, with the title “Health informatics – Electronic health record communication – Part 1: Reference model”. Its recent publication (2008), as well as the equally recent publication of other standards by ISO (ISO 17090-3:2008; “Health informatics – Public key infrastructure – Part 3: Policy management of certification authority “; ISO 11073-90101:2008; “Health informatics – Point-of-care medical device communication – Part 90101: Analytical instruments – Point-of-care test”) demonstrate on the one hand the stakes of the exchange of healthcare data, and on the other hand the need for coherence between the various standards.
This standard CEN prEN 13606 is made of four volumes [EHC 03], respectively dealing with:
– the extended architecture, which describes the architectural components: the file, to keep a person’s health data under a digital format, and the file’s components, including:
- compositions, dependent on the place and the moment of care (e.g.: home visit report, radio exam results, etc.),
- directories which group the data concerning a person’s health through time, or the data linked to a specific problem (a child’s personal health record),
- the data’s visual synthesis (list of health problems, growth curb),
- the links necessary to connect two file components (cataract – [aggravating factor]- diabetes; hepatic biopsy – [record of]-jaundice);
– the list of field terms provides tables of names and values which can be used to categorize the above components;
– the distribution rules define the rules for security and for the access to the personal file (who: the family doctor; why: medical certificate needed for sports, etc.);
– the messages for the exchange of information, message of file request, transfer message, notification of the exchange’s status.
The standardization works are still ongoing. Thus, the technical committee ISO TC 2155, dedicated to computer sciences in the healthcare field (Health informatics) features workgroups on the following themes:
– data structure;
– data exchange;
– semantic content;
– security;
– health cards;
– pharmacy and medicines business;
– business requirements for Electronic Health Records.
Within the structure of the CEN/TC 251 Working Group IV, “Technology for Interoperability”, we find such themes as6:
– interoperability of healthcare multimedia report systems;
– interoperability of medical devices within acute care units;
– evaluation of physiological analysis systems;
– healthcare information system architecture.
These works standardize the exchanges and/or the mediums of health data. Thus, if the EHRcom standard offers a message perspective, the CDA (Clinical Document Architecture), on the other hand, offers a document perspective.
A document model helps elaborate a shared medical file as much as a personal card. For example, the CDA does not enforce a particular medium or a physical architecture. Moreover, for people in temporary need of mobility, such a solution allows the downloading of some of the shared medical file onto cards, which those persons can carry on them.
7.5.2.4. The SNOMED nomenclature
Beyond the structure of the messages and documents, the communicated data must have the same, non-ambiguous meaning for the systems which exchange or share information. This pertains to semantics and terminology. It is the goal of the SNOMED (Systematized Nomenclature of Medicine) project, a multiaxial, hierarchical classification system, featuring 364,000 concepts7. It covers the greatest part of medical data, such as diseases, semiology, protocols, and pharmaceutical components.
It allows for the indexing, storage, classification and organization of the contents of medical records.
These hierarchies include [CAP 07]:
– the clinical findings represent the determined trouble, the agent responsible for it, its severity, etc.;
– the procedure explains how to treat the trouble, with a differentiation between invasive and non-invasive procedures, for example biopsy or excision, but also the technique used, etc.;
– the specimen characterizes the collected specimen (urine, etc.), as well as its morphology (cyst, abscess, etc.);
– the body structure specifies the concerned structure (thyroid gland, stomach, etc.) and positions in terms of laterality (left, right, right and left, unilateral, etc.);
– the pharmaceutical or biologic products characterize the active ingredient, the dosage, etc.;
– the situation with explicit context indicates that a medical recording is affected by the context of said recording ([CAP 07], p. 4-24): indeed, “breast cancer” can be used to describe a family history of breast cancer, a personal history of breast cancer, and finally the actual diagnosis of breast cancer;
– the events define the temporal dimension of clinical characteristics (occurrence, sequence, etc.);
– the physical force characterizes mechanisms of injury;
– the physical object characterizes man-made objects, such as a pair of rubber gloves, an artificial kidney, an implant;
– the observable entity is used to describe what can be observed, without it being a finding, e.g. the type, the age;
– the environments and geographical locations concern the places (a country, a region), the premises (a unit of intensive care);
– the social context concerns the social conditions which can impact health, such as family status, work, lifestyle;
– the organism characterizes a living organism, for example a virus, a bacteria, a mycosis, etc.;
– the substance helps characterize components such as food or chemical allergens, toxicity or dental porcelain material;
– the staging and scales are used to describe phenomena, such as the Stanford-Binet Intelligence scales, the Glasgow coma scale, obstetrics staging;
– the linkage concept helps define relationships, associations, such as link assertions;
– the qualifier value helps characterize an element, a phenomenon (strong, soft, bitter, etc.);
– the record artifact provides information, such as ECGs, EEGs, etc.
If the elaboration of ontology in the medical field, which would enable the semantic interoperability of information systems, is necessary, such a medical ontology could not cover the subtleties of human communication.
Indeed, such ontology used by a data treatment system, does not take into account cultural aspects, source of variations, or the pragmatic dimension typical of human communication.
To be useful to health professionals, the information systems must feature labels and data which those professionals understand, control and manipulate. Information systems often differ.
Such ontology has the quality of being a pivot language, a tool for the correspondence of various information systems.
Whatever the chosen technological solution, it will not be able to take into account and express the richness of human communication.
7.5.2.5. An example of appropriation and implementation
If standardization is a necessary stage, it must be completed through local, regional, national or even international actions, with medical and paramedical agents implementing standards, leaning on tools which respect these standards, and through the industrialists, who design their systems in conformity with these standards.
These are the goals and activities of the ENOSIS (Echanges Normalisés, Organisés et Sécurisés des Informations en Santé – Standardized, Organized and Secured Exchanges of Health Data) project [ENO 08]. This association regroups 15 healthcare networks.
The objectives of the ENOSIS group [ENO 08] are:
– “to inform the networks’ agents, and healthcare professionals in general, the industrialists of medical computer sciences, and the institutions, on the importance of adopting communication standards in the healthcare field;
– to standardize the cards or files of the group’s networks into messages, while following the standards recommended by the standardizing structures, and develop tools that will assist standardization;
– to create common specifications, and develop a client and exchange server, standardized, organized and secure, for the health data meeting said specifications. These products’ architecture is modular, so as to help the existing tools adopt those standards.”
In this context, the ENOSIS group develops a server of standardized, secure messages, as well as client software [ENO 08], by leaning on the HERcom standards (for example CEN prEN 13606) and MMF/XMF for the compatibility with the Sentinel service of Cégétel.rss (secure medical messaging). Finally, in order to uphold the security of personal medical data, the ENOSIS project uses the professional health card (CPS, Carte Professionnelle de Santé, Professional Health Card) and calls on the services of the CPS GIP (Groupement d’Intérêts Publiques, Grouping of Public Interests), such as the phonebook, the revocation list, the publication of public keys.
The aforementioned requirements on coordination (section 7.4) are met through a system of collaboration. Collaboration consists of a sequence of requests/replies between two or more agents in the network, a supplier and an applicant.
Moreover, several collaborations between different agents can be grouped within a single process ([ENO 08], section “The ENOSIS approach”). Collaborations may be modeled in terms of Conversation for action following the model of language acts ([ENO 08], section “Enosis. Work flow and exchange modeling” and “Collaborations and processes: the structuring concepts of the organization of communication, following the Enosis approach”).
From the standpoint of the doctor, agent within a network, the tools developed within the ENOSIS project will help him ([ENO 08], section “The ENOSIS approach”):
– choose a card model among the models designed by the network;
– write down the data within a form corresponding to that model, from a browser, offline or online;
– securely send the filled-in form to the coordinator or another network member (an Internet connection is then imperative);
– securely consult the cards which have been sent to him, or concern one of his patients (on the condition that the network is managing that particular care relationship);
– get a visual of the operating statistics, subject to rights of access;
– export all or part of the database’s files, depending on the access rights, in order to run the medical data through particular statistical treatments within an adapted software (Excel, Access, SPSS, Statistica, etc.).
An experiment in actual use was led with the digital personal health records of children.
The results ([ENO 08], section “The ENOSIS approach”) show that:
– very strict protocols and a highly ergonomic interface are needed for the parents and the delegation to control confidentiality;
– the use of the CPS seems necessary to authenticate the liberal health professionals, considering the potential scope of the health record’s use;
– the coexistence of both the paper and digital personal health record must be managed in a flexible, economical way, which is still to be designed;
– in daily use, the real-time data entry will require the use of some technologies which are still quite new (tablet PC, Wifi);
– the data entry must be possible offline;
– to avoid doubles, the personal software of health professionals will have to be able to interoperate with the personal health record;
– as a shared health record centered around the patient, the personal health record will undergo coherence reviews to ensure the quality of the recorded data;
– end control and use assistance functionalities will be found within the professional software;
– the personal health record must evolve easily in order to accept branches specific to the needs of the healthcare networks using it, and the structure of its data will also have to be standardized.
Moreover, this approach is also implemented within the project “ReSOP Interoperability”, aimed at creating a healthcare network for pediatric oncology. “The goal is to improve the continuity and quality of the care through the sharing of a therapeutic project and a coordinated coverage of both the children and his family, on the medical, paramedical, psychological and social levels” ([ENO 08], section “The ENOSIS approach”). “The project “ReSOP Interoperability” consists of implementing the necessary technical infrastructure for the digital transfer of the hospital-town and town-hospital liaison cards within the ReSOP healthcare network” ([ENO 08], section “the ENOSIS approach”).
7.6. Difficulties encountered
Implementing information technologies is not easy when a service must be provided from end to end, to manage and store patient-related data and keep them for the duration of the patient’s life.
The first difficulty lies in the specific characteristics of medical activities. Coordinating the activities of all the medical and paramedical agents, and relying on the coordination of their information systems, considering the characteristics of these activities which we have previously identified, can only be managed through the implementation of solutions already used in the field of process automation. It is crucial to take into account the character, both eminently dynamic and contingent, of these activities, something which is not currently possible with the concepts, methods and tools of process modeling. Consequently, studies must be led, on the one hand, to develop concepts and methods able to take these characteristics into account, and on the other hand, to develop tools adapted to these new concepts and these new methods.
The second difficulty lies in the transition between paper and digital files. For each patient, the doctors and health facilities already have a set of data within paper files. Several solutions exist. The first would consist of digitalizing the paper data in order to create an image of these pages. The results of this kind of digitizing are however hard to manipulate, classify and research. The solution which would consist to digitalize such documents using optical character recognition technology is not more conclusive. Most documents are manuscript and the character recognition performances are limited. Still, this technology would enable plain text searching in digitalized documents, hence facilitating their classification and helping easy research of pertinent documents. Managing documents both in paper and digital form is not more appealing. First, the coherence must be upheld between the two mediums, including the patient’s unique identification, and one must know beforehand on which medium to look for the required data. The search time must take into account the fact that the research procedures depend on the medium and require various cognitive skills.
The third difficulty lies in the necessity of keeping the digital data available and readable during the patient’s entire life, and beyond. Indeed, in the event of organ transplants, Knowledge of the donor’s clinical history is essential in order to identify a possible contamination. The recent trial concerning the growth hormone demonstrated the risks of contamination, in that particular case contamination by a prion, and the necessity to keep a record of medical procedures. The physical medium (floppy disks of various formats, USB key, etc.) evolves, along with binary coding, the operating system on which the data are stored, the files’ formats, the application which will read those files, the meaning of the data stored in the files, etc. As soon as major evolutions happen, the old data must be transferred onto the new mediums, and their completeness, integrity, privacy or confidentiality must be guaranteed. This requires organization, planning, budget, the implementation of specific resources, and the transfer to be monitored, to make sure there is no loss or corruption of data, etc.
Finally, a tool must be designed to store the data not correctly transferred. Since the probability that all data will be synchronously transferred is low, the new mediums must be compatible and able to interoperate with the old ones. But should all this information be kept during the person’s entire life, or should one only keep a certain number of pertinent, meaningful data? If all data must be stored, the volume will be very large, which pleads the cause of limited storage of pertinent data. But determining the importance of such or such information is just as complicated. Data sometimes only becomes meaningful much later on, with new information, new means of investigation.
The fourth difficulty lies in the confidentiality of the personal medical data, as well as the patient’s access to the featured information. These requirements on the confidentiality of and access rights to the medical data are framed by a set of legal texts. Their implementation relies on the standards and regulations on the security of information systems, introduced in Chapter 12, “Standardization in the field of systems and systems of systems engineering”. Beyond those legal and technical dimensions, the questions about confidentiality and access rights have a particularly important societal dimension and, therefore, are treated in information documents, such as the thematic file “Patients’ rights: access to the medical record” (“Droits des malades: accès au dossier médical”) and the document “the expectations of patients and people covered by health insurance about health information systems” (“les attentes des patients et des assurés en matière de systèmes d’information de santé”), published by the CISS8 [CIS 07]. This aspect also has a non-negligible financial dimension, as attested by Google and Microsoft’s offers about a service for the storage of medical data9.
In France, the GIP DMP10 is in charge of the patient file project. Lastly, providing all the medical and paramedical agents with secure systems of medical data entry, reading and communication, may have a non-negligible cost.
7.7. Conclusion
In the medical field, capability challenges led to the design of systems of systems, healthcare networks, including health facilities, private practices, but also paramedical and social agents. Providing end-to-end services, focused on the patient, requires those agents’ activities to be coordinated, and patient-related data to be exchanged, with security requirements typical of personal data. The diversity of the information systems implemented to support these activities requires them to interoperate in order to achieve such coordination, an interoperability which must be largely built on the standards of the medical field.
In such a context, the main difficulties lie in the expression and modeling of the medical activities, which are always the “here and now” product of the interaction between health personnel and patients, in the transition between paper and digital mediums, the necessity of keeping these data available during the patient’s entire life, and finally, in the control of the personal data’s confidentiality.
7.8. Acknowledgments
I warmly and most particularly would like to thank (in alphabetical order) Karima Bourquard, Yves Constantinidis, Claude Pourcel, Jean-Claude Sarron, Michel Veret, who were large contributors to this chapter.
I would also like to thank the many people who helped me with this document and the many people whom I was able to converse with, and whom I could not give an exhaustive list of, but who will not fail to recognize themselves.
7.9. Bibliography
[ABE 05] ABE T., “What is Services Science?”, Research Report, n° 246, The Fujitsu Research Institute, 2005.
[AMA 09] AMALBERTI R., “Violations et migrations ordinaires dans les interactions avec les systèmes automatisés”, Journal Européen des Systèmes Automatisés, vol 43/6, pp.647660, 2009.
[BRI 05] BRIQUET M., COLIN J., GOURC D., Pourcel C., “Organisation d’un système hospitalier par pôle d’activité: modélisation et identification des problèmes de pilotage”, Actes du 6e Congrès International de Génie Industriel, Besançon, June 2005.
[BRO 99] BROWNING T., “Designing System Development Projects for Organizational Integration”, Systems Engineering, vol. 2, n° 2, 1999.
[CAP 07] COLLEGE OF AMERICAN PATHOLOGISTS, SNOMED Clinical Terms User Guide, 2007, available online: http://www.ihtsdo.org/our-standards/technical-documents.
[CIS 06] CISS, “Les attentes des patients et des assurés en matière de systèmes d’information de santé”, 2006, available online: http://www.leciss.org/.
[CIS 07] CISS, “Droits des malades: accès au dossier médical”, thematic sheet of the CISS n°11, available online: http://www.leciss.org/, 2007.
[DAG 04] DAGNINO G.B., “Complex systems as key drivers for emergence of a resource-and-capability-based interorganizational network”, Emergence: Complexity & Organization, vol. 6, n° 1-2, 2004, available online: http://iscepublishing.com/ECO/about_eco.aspx.
[EHC 03] EHCR, “Introduction à ENV 13606”.
[ENO 08] ENOSIS, information taken from the site (now closed) http://enosis.phpnet.org/, 2008.
[FID 06] FIDOCK J., “Organisational Structure and Information Technology (IT): Exploring the Implications of IT for Future Military Structures”, DSTO, Edinburgh, 2006.
[GIU 01] GIUSIANO B., “La communication dans les réseaux de soins”, XVe Journée de Dermatologie Pédiatrique, Arles, 2001.
[GMS 06a] GMSIH, “Architecture et urbanisation des SIPS; Exemple d’architecture métier -Commentaires”, 2006, available online: http://www.gmsih.fr/.
[GMS 06b] GMSIH, “Architecture et urbanisation des SIPS; Exemple d’architecture fonctionnelle cible”, 2006, available online: http://www.gmsih.fr/.
[GMS 07a] GMSIH, “Etude de définition relative au système d’information pour la coordination des soins entre les réseaux de santé, la médecine de ville, le secteur médico-social et les établissements de santé”, 2007, available online: http://www.gmsih.fr/.
[GMS 07b] GMSIH, “Rapport de la première campagne d’évaluation BREC; transversalité et schéma directeur du système d’information”, 2007, available online: http://www.gmsih.fr/.
[GMS 07c] GMSIH, “Enquête sur la situation des Systèmes d’Information Hospitaliers dans les établissements de santé”, 2006, available online: http://www.gmsih.fr/.
[GOF 79] GOFFMAN E., Asiles, Les Editions de Minuit, Paris, 1979.
[HAR 02] HARADEN C. & AMALBERTI R., Course: What is New in Safety Thinking and its Implications for Health Care, IHI forum, London, UK, 2002.
[HID 06] HIDAKA K., “Trends in Services Sciences in Japan and Abroad”, Science and Technology Trends, Quarterly Review, n° 19, 2006.
[LER 09] LEROY N., CHAZARD E., BEUSCART R., BEUSCART-ZÉPHIR M.C., “Toward automatic detection and prevention of adverse drug events”, Stud. Health Technol. Inform., vol. 143, p. 30-35, 2009.
[MIN 82] MINTZBERG H., The Structuring of Organizations, Prentice Hall, 1979.
[PEL 09a] PELAYO S., ANCEAUX F., ROGALSKI J., BEUSCART-ZÉPHIR M.C., Organizational vs. technical variables: impact on the collective aspects of healthcare work situations, Stud. Health Technol. Infrom., vol. 150, p. 307-11, 2009.
[PEL 09b] PELAYO S., BERNONVILLE S., KOLSKI C., BEUSCART-ZÉPHIR M.C., “Applying a human factors engineering approach to healthcare IT applications: example of a medication CPOE project”, Stud. Health. Technol Inform., vol. 143, p. 334-339, 2009.
[PER 84] PERROW C., Normal Accidents, Doubledays, New York, 1984.
[POU 06] POURCEL C., CLÉMENTZ C., “Approche modulaire pour l’aide à la conception de l’organisation d’un système de production de soins”, Actes de la conférence Gestion et Ingénierie des Systèmes Hospitaliers (GISEH), Luxembourg, September 2006.
[POU 08] POURCEL C., CLÉEMENTZ C., BISTORIN O., “Système productif de soins de secours, d’urgence et 2HM; approche systèmes de systèmes”, documents personnels, 2008.
[RAK 05] RAKOTONDRANAIVO A., GRANDHAYE J.P., POURCEL C., “Identifications des décisions dans un réseau de santé”, Actes du 6e Congrès International de Génie Industriel, 2005.
[ROJ 03] ROJOT J., Théories des organisations, Editions Eska, Paris, 2003.
[SPO 06] SPOHRER J., MAGLIO P., The Emergence of Service Sciences: Toward Systematic Service Innovations to Accelerate Co-creation of Value, IBM Almaden Research Center, San Jose, 2006.
[THO 04] THOMPSON J., Organizations in Action, Transaction Publishers, New Brunswick, 2004, first edition 1967.
1 Chapter written by Jean-René Ruault.
1. CNIL: Commission nationale de l’informatique et des libertés (French Data Protection Authority).
2. The current life expectancy of a French citizen is higher than 81 years old, according to the numbers published in March 2008.
3. RFID (Radio Frequency IDenfication): this type of chip is associated with an antenna and the set constitutes a radio frequency tag, a small object enabling the reception of and answer to radio requests sent by a transceiver.
4. CME: Commission médicale de l’établissement (Facility Medical Commitee).
5. Website: http://www.iso.org/iso/standards_development/technical_committees.
6. Website: http://www.tc251wgiv.nhs.uk/pages/work.asp>.
7. Website: http://www.nbirn.net/research/ontology/snomed.shtm (downloaded on March, 4 2008).
8. Interassociative collective on health (http://www.leciss.org/).
9. Advertisement “Google présente un service de stockage des données médicales”, published February 29th, 2008 (http://fr.news.yahoo.com/rtrs/20080229/ttc-google-sante-fe50bdd.html) and “Les dossiers médicaux personnels, nouvel enjeu pour Google et Microsoft” (http://fr.news.yahoo.com/afp/20080302/thl-usa-internet-sante-96993ab.html).
10. GIP: Grouping of Public Interest; DMP: Personal Medical File.
